Exercise and diet alone often fails to effectively treat people with extreme and excessive obesity. Bariatric surgery is an operation that is performed in order to help such individuals lose weight. Evidence suggests that bariatric surgery may lower death rates for patients with severe obesity, especially when coupled with healthy eating and lifestyle changes after surgery.
Principles of bariatric surgery
The basic principle of bariatric surgery is to restrict food intake and decrease the absorption of food in the stomach and intestines.
The digestion process begins in the mouth where food is chewed and mixed with saliva and other enzyme-containing secretions. The food then reaches the stomach where it is mixed with digestive juices and broken down so that nutrients and calories can be absorbed. Digestion then becomes faster as food moves into the duodenum (first part of the small intestine) where it is mixed with bile and pancreatic juice.
Bariatric surgery is designed to alter or interrupt this digestion process so that food is not broken down and absorbed in the usual way. A reduction in the amount of nutrients and calories absorbed enables patients to lose weight and decrease their risk for obesity-related health risks or disorders.
Body mass index (BMI)
Body mass index (BMI), a measure of height in relation to weight, is used to define levels of obesity and help determine whether bariatric intervention is required. Clinically severe obesity describes a BMI of over 40 kg/m2 or a BMI of over 35 kg/m2 in combination with severe health problems.
Health problems associated with obesity include type 2 diabetes, arthritis, heart disease, and severe obstructive sleep apnea. The Food and Drug Administration (FDA) approves the use of adjustable gastric banding for patients with a BMI of 30 kg/m2 or more who also have at least one of these conditions.
Types of Bariatric Surgery
There are various types of bariatric surgeries that can be performed. Surgery may be performed using an “open” approach, which involves cutting open the abdomen or by means of laparoscopy, during which surgical instruments are guided into the abdomen through small half-inch incisions. Today, most bariatric surgery is laparoscopic because compared with open surgery, it requires less extensive cuts, causes relatively minimal tissue damage, leads to fewer post-operative complications and allows for earlier hospital discharge.
There are four types of operations that are offered:
- Adjustable gastric banding (AGB)
- Roux-en-Y gastric bypass (RYGB)
- Biliopancreatic diversion with a duodenal switch (BPD-DS)
- Vertical sleeve gastrectomy (VSG)
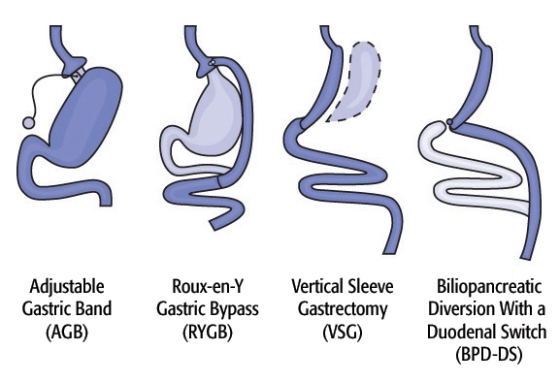
Diagram of Surgical Options. Image credit: Walter Pories, M.D. FACS.
Each of the surgery types has advantages and disadvantages and various patient factors affect which procedure is chosen including BMI, eating habits, health problems related to obesity, and number of previous stomach surgeries. The patient and provider should discuss the most suitable option by considering the benefits and risks of each type of surgery.
Surgical and post-operative risks
People who have had bariatric surgery need to adhere to a rigorous and lifelong diet and exercise plan to prevent complications and to avoid putting on weight after surgery. In addition, patients may develop excess loose and folded skin that requires further surgery to remove and tighten.
As with all types of surgery, bariatric surgery is associated with risks including internal bleeding, deep vein thrombosis, infections, and pulmonary embolism (blood clot in the lungs). It is estimated that the risk of dying shortly after bariatric surgery is around 1 in 200.
References
- http://www.nhs.uk/conditions/weight-loss-surgery/Pages/Introduction.aspx
- https://www.niddk.nih.gov/health-information/weight-management/bariatric-surgery
- https://med.virginia.edu/
- https://www.siumed.edu/
- http://www.lapsf.com/bariatricsurgery.pdf
- https://louisville.edu/medschool/gimedicine/division-lecture-files/marsano-lectures/bariatric%20surgery.pdf
Further Reading
Last Updated: Jun 19, 2023