What is a punch biopsy?
A punch biopsy is a medical procedure used to remove a small, cylindrical piece of skin for laboratory examination, usually through tissue culture or microscopy. This procedure is typically done under local anesthesia and provides a full-thickness sample of skin, which is essential for diagnosing a variety of skin conditions. Punch biopsy is generally considered a relatively low-risk procedure and is often performed to investigate lesions that cannot be diagnosed through visual inspection alone.

Image Credit: Anamaria Mejia/Shutterstock.com
The biopsy is done using a specialized tool, a tube-shaped instrument with a sharp blade. The tool, which ranges in size from 1 mm to 8 mm, is rotated through the skin to remove a small sample. The sample is then sent for microscopic examination to identify underlying issues like infections, inflammatory conditions, or cancer.
Why is a punch biopsy done?
A punch biopsy is primarily performed to diagnose skin conditions that cannot be assessed definitively based on their outward appearance alone. It is an essential tool in cases where further investigation is needed, offering a reliable way to confirm or rule out various conditions.
- Suspicious skin lesions: One of the most common reasons for conducting a punch biopsy is to assess suspicious growths or lesions, especially those that may suggest skin cancer, including non-melanoma types like squamous cell carcinoma (SCC) and basal cell carcinoma (BCC), or melanoma. In such cases, the biopsy helps to distinguish malignant cells from benign growths, leading to timely diagnosis and appropriate treatment.
- Inflammatory and infectious conditions: Punch biopsies are also useful for diagnosing inflammatory skin disorders such as eczema and psoriasis or autoimmune diseases like lupus erythematosus. The biopsy provides full-thickness samples, which help assess deeper layers of the skin and determine the exact nature of the inflammation or infection.
- Full-thickness assessment: One key advantage of a punch biopsy is its ability to sample all layers of the skin. This makes it particularly valuable when diagnosing conditions that may affect the deeper layers, such as scarring alopecia, blistering eruptions like bullous pemphigoid, or sarcoidosis.
By providing clear and detailed histopathological findings, a punch biopsy is essential in determining the cause of unexplained skin changes, helping doctors make accurate diagnoses that may otherwise be difficult through visual inspection alone.
Preparing for a punch biopsy
Before undergoing a punch biopsy, several essential steps help ensure the procedure runs smoothly and the results are reliable:
- Informed consent and documentation: The patient must consent to the biopsy procedure. Photography should be used to document the site of the biopsy and the lesion of interest for reference and accurate diagnosis.
- Medication management: The healthcare provider evaluates whether the patient should temporarily discontinue medications such as blood thinners. In most cases, patients on anticoagulants can continue their medications, as punch biopsies are minimally invasive, and hemostasis can be achieved easily.
- Skin preparation: The patient’s skin is cleansed with povidone-iodine solution. Afterward, a local anesthetic (typically 2% lidocaine with epinephrine) is injected into the biopsy area using a 30-gauge needle, ensuring minimal discomfort during the procedure.
- Biopsy area selection: The most abnormal-appearing part of a lesion is typically selected for biopsy. Ideally, the biopsy is done on the edge of an actively growing lesion to ensure the sample is representative of the disease process.
- Skin tension and lines of least resistance: To minimize cosmetic scarring, the lines of least skin tension should be identified. For instance, in arms, these lines generally run perpendicular to the length of the extremity.
- Step-by-step biopsy: The punch biopsy instrument is held vertically, and a twirling motion rotates it downward. Once the blade reaches the dermis and subcutaneous fat, the instrument is removed, and the specimen is elevated carefully. Forceps are used minimally to avoid crush artifacts, and the specimen is placed in the appropriate transport medium.
- Suturing: In larger biopsies (over 2 mm), a suture is applied to close the wound and prevent excessive scarring. Stitches are commonly done using 5-0 nylon in most non-facial areas and 6-0 nylon for facial areas.
Steps of the punch biopsy procedure
Here are the key steps involved in performing a punch biopsy:
- Patient consent and documentation: Obtain informed consent and document the lesion site with photography.
- Skin cleansing and anesthesia: Cleanse the area with a disinfectant (usually povidone-iodine) and inject local anesthesia.
- Positioning: Stretch the skin in perpendicular lines to the skin's natural tension lines. This ensures better healing and minimal scarring.
- Biopsy insertion: The punch biopsy instrument is inserted perpendicularly and rotated through the skin’s layers until it reaches the subcutaneous fat.
- Specimen removal: After obtaining the specimen, it is carefully elevated with forceps and cut at the base using scissors.
- Suturing (if needed): Suture the site (for biopsies over 2 mm) to facilitate proper healing.
- Post-procedure care: Antibiotic ointment and bandages are applied. A follow-up appointment is scheduled to review the results.
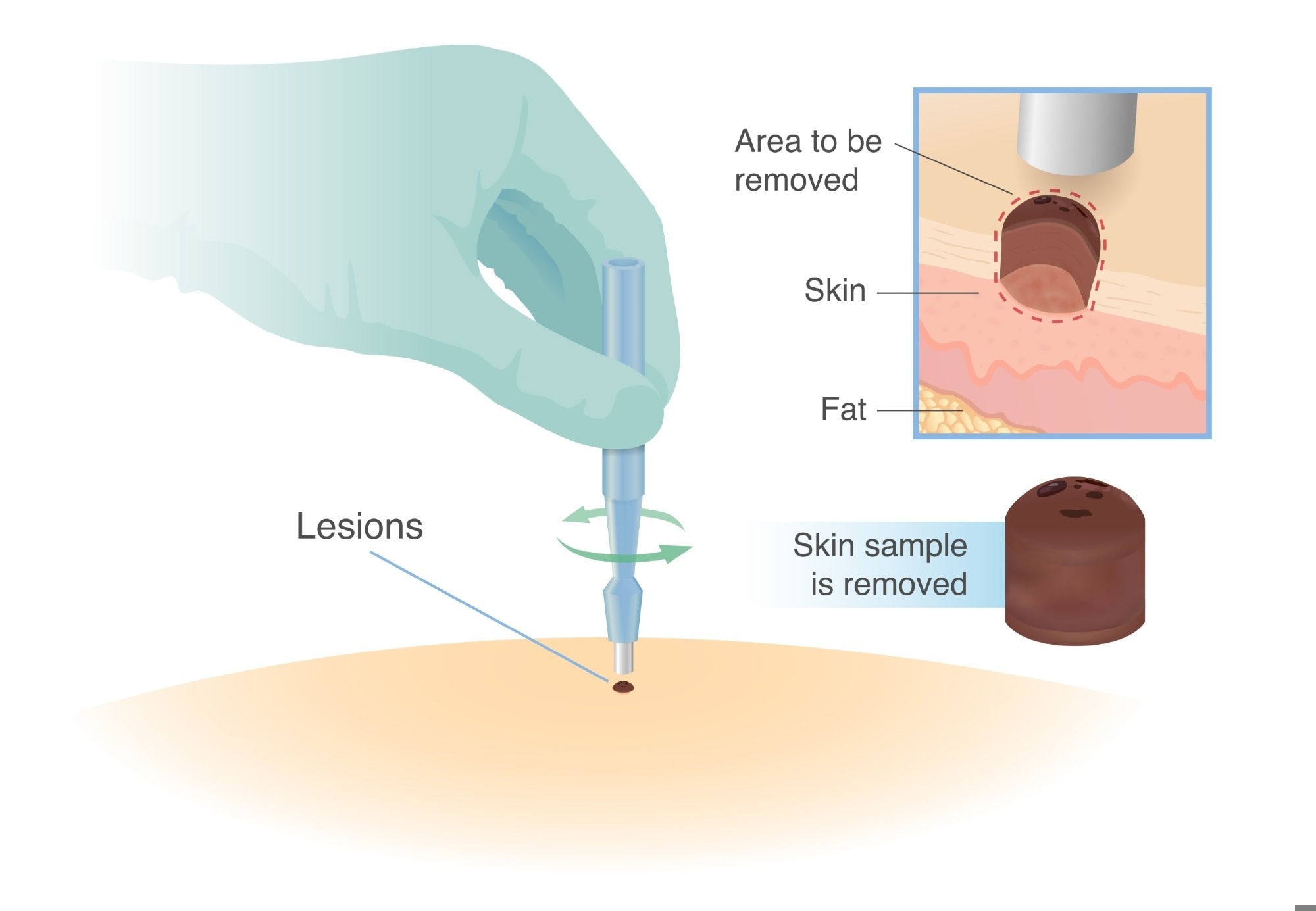
A medical illustration depicting a punch biopsy procedure, where a circular tool is used to remove a small skin sample for diagnostic analysis. The diagram highlights the lesion, the area to be removed, and the extracted skin sample. Image Credit: solar22/Shutterstock.com
Risks and precautions of punch biopsy
While a punch biopsy is generally safe and considered a low-risk procedure, there are still some potential risks and precautions to consider:
- Infection: As with any invasive procedure, infection is a risk, though it is rare.
- Bleeding: If patients have a bleeding disorder, extra precautions should be taken.
- Cosmetic concerns: There may be some scarring or changes in pigmentation, especially with larger biopsies. Locations like the face are more susceptible to visible scars.
- Nerve injury: The biopsy may injure nerves, especially on the face and extremities. Special care should be taken to limit instrument depth in such cases.
- Inaccurate results: In some rare cases, inadequate sample size or poor orientation of the sample may lead to inaccurate diagnoses.
Patients should be informed about potential complications and know when to contact their healthcare provider.
Recovery and aftercare
The recovery from a punch biopsy is typically swift, but some aftercare is necessary for optimal healing and to reduce the risk of complications:
- Follow-up: After the biopsy, a follow-up visit is recommended to remove sutures and review biopsy results.
- Wound care: Keep the biopsy site clean and dry for the first few days. A bandage should be worn for protection, and antibiotic ointment may be applied to prevent infection.
- Signs of infection or Complications: Watch for symptoms of infection, including increased redness, swelling, pain, or discharge. In case of excessive bleeding or these signs, contact the healthcare provider.
- Sutures and scar management: Once stitches are removed, apply scar ointments as directed to minimize cosmetic effects.
References
- http://www.nhs.uk/conditions/Biopsy/Pages/Introduction.aspx
- https://www.gosh.nhs.uk/
- http://www.cancer.ca/en/cancer-information/diagnosis-and-treatment/tests-and-procedures/punch-biopsy/?region=on
- Zuber T. J. (2002). Punch biopsy of the skin. American family physician, 65(6), 1155–1164.
- Wark, K. J., Smith, S. D., & Sebaratnam, D. F. (2020). How to perform a skin biopsy. The Medical journal of Australia, 212(4), 156–158.e1. https://doi.org/10.5694/mja2.50473
- Greenwood, J. D., Merry, S. P., & Boswell, C. L. (2022). Skin biopsy techniques. Primary Care: Clinics in Office Practice, 49(1), 1–22. https://doi.org/10.1016/j.pop.2021.10.001
Further Reading
Last Updated: Feb 13, 2025