Niacin, which is otherwise known as vitamin B3, is essential to proper cell functioning.

Image Credit: Olga Chernyak / Shutterstock.com
Niacin is involved in energy metabolism as part of reduction/oxidation coenzymes, the metabolism of amino acids, as well as in detoxification reactions for drugs and other substances. It also represents an important therapeutic option for several conditions.
A lack of niacin can result in a disease called pellagra. This condition has been common throughout human history, namely among impoverished people whose diet consisted almost entirely of corn products. This type of diet lacks an adequate amount of niacin, thus triggering in turn symptoms such as diarrhea, inflamed mucous membranes, skin sores, weakness, irritability, and mental delusions.
Biochemistry of niacin
Niacin is a colorless and water-soluble derivative of pyridine, with a carboxyl group found at the 3-position. This essential vitamin comes in several forms, namely nicotinic acid (pyridine-3-carboxylic acid) and nicotinamide (nicotinic acid amide); however, there are also some other derivatives that exhibit the biological activity of nicotinamide as well, such as inositol hexanicotinate.
Due to their similarities in biochemical activity, the terms niacin, vitamin B3, nicotinic acid, and nicotinamide are often used interchangeably. In the human body, nicotinic acid and its derivative nicotinamide are converted to nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP). Both NAD and NADP are coenzymes that are necessary for hundreds of oxidation-reduction redox reactions, which are essential sources of energy for a myriad of cellular functions.
NAD is necessary for the synthesis of deoxyribonucleic acid (DNA), and is also involved in transferring chemical components to proteins. Such transfers can be catalyzed by poly-ADP-ribose-polymerases (PARPs), which regulate the transfer of adenosine diphosphate (ADP)-ribose units from NAD to proteins. Several ongoing research projects continue to explore the numerous functions of niacin and PARPs, as well as their mutual interplay in health and disease.
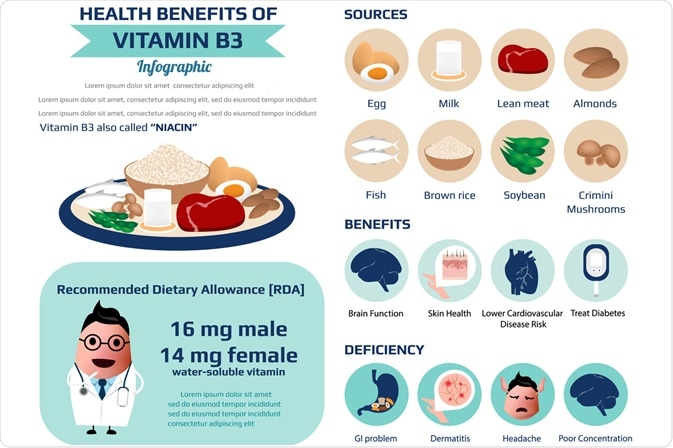
Image Credit: nipada_hong / Shutterstock.com
Effects on the human body
Niacin has a plethora of beneficial effects for the human organism, especially regarding the metabolism of cholesterol and lipoproteins. There is a considerable amount of evidence on how niacin improves lipid profiles and reduces vascular disease, which has thus prompted its use in the treatment of cardiovascular diseases.
It has been repeatedly shown that niacin lowers triglycerides and low-density lipoproteins (LDL), which are often referred to as “bad” cholesterols. Niacin also simultaneously raises high-density lipoprotein (HDL) levels, which are considered “good” cholesterol, with a subsequent effect on plaque and thickness of arterial walls. Furthermore, this essential vitamin also decreases the plasma concentration of lipoprotein A, which plays an independent role in the development of coronary heart disease.
Much of the aforementioned changes take place in the liver and influence the way in which this organ handles cholesterol, triglyceride, and lipoprotein metabolism. Niacin inhibits a specific liver enzyme involved in the synthesis of triglycerides, thus resulting in lower levels of triglycerides. It also lowers the expression of the beta-chain of ATP synthase, which is another liver chemical, subsequently increasing HDL levels by decreasing its breakdown.
Some studies have reported several non-lipoprotein mediated effects of niacin with an effect on atherosclerosis progression and risk. In addition to the favorable lipoprotein modulating effects of niacin, pharmacological studies have revealed its anti-inflammatory effects in macrophages, adipocytes, and vascular endothelium.
Niacin also lowers the expression of cytokines that are involved in building up cholesterol-filled plaques in arterial walls. Restraint of immune cell infiltration of the vessel wall is mediated by GPR109A, which is a receptor for niacin and the commensal metabolite butyrate, which subsequently retards atherogenesis in the absence of significant lipid changes.
References
Further Reading
Last Updated: Jan 16, 2023