Beta-lactam antibiotics are the most commonly prescribed group of drugs, sharing together a specific structural feature of the beta-lactam ring. Among them, penicillin is one of the earliest discovered and most widely used antibiotic agents. In addition, penicillin is regarded as one of the safest and most efficacious antimicrobial drugs.
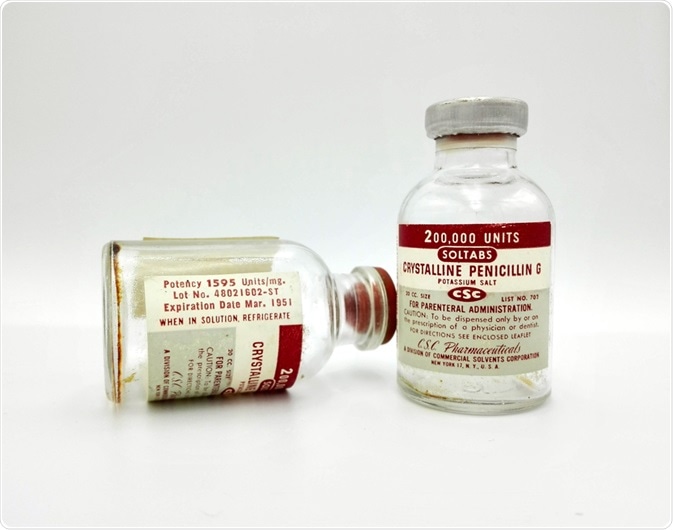
Image Credit: Walter Cicchetti / Shutterstock.com
The discovery of penicillin
The development of penicillin altered the entire direction of approaches to treating infectious diseases and saved the lives of millions of people. In August 1928, Alexander Fleming came back from a vacation to his usually disordered and messy laboratory. In one of the Petri dishes, he accidentally noticed an unusual phenomenon: separate colonies of staphylococci and, adjacent to the dish's edge, a colony of mold about 20 millimeters (mm) in diameter.
This discovery was dormant for some time before other researchers took up the challenge to further explore its clinical possibilities. Two investigators at Oxford, Howard Florey and Ernst Chain, conveyed the inherent potential of penicillin for medical use and, along with Fleming, shared the 1945 Nobel Prize for Medicine.
If Alexander Fleming did not stumble across this discovery, our antimicrobial armory available today would have been significantly different and, for some time, we would have to rely solely on highly developed varieties of sulphonamides or similar, synthetic, and non-antibiotic antibacterial agents.
The accident that changed the world - Allison Ramsey and Mary Staicu
Structure and nomenclature
Penicillin was initially extracted from the species of the mold called Penicillium notatum. A mutant of a related mold, Penicillium chrysogenum, was later found to give the highest yield of penicillin and was subsequently used for the commercial production of this antibiotic.
The basic structure of all the penicillins consists of a thiazolidine ring fused with a beta-lactam ring, creating a fundamental nucleus (also known as 6-amino penicillanic acid) that is crucial for their antibacterial activity. A plethora of semisynthetic penicillins is produced by altering the composition of the side chains attached to this nucleus.
Powerful electron-attracting groups attached to the amino acid side chain can prevent an acid attack. A bulky group attached to the amino acid side chain results in steric hindrance which, in turn, interferes with the enzyme attachment that can possibly deactivate the penicillins (for example, methicillin). If the polar character of the compound is increased, as is the case with ampicillin or carbenicillin, a greater activity against Gram-negative bacteria can be observed.
The penicillins are chemically described as 4-thia-1-azabicyclo (3.2.0) heptanes. In order to simplify the unsubstituted bicyclic ring system, which is the core skeleton of penicillin, it was given the name “penam.” Accordingly, the penicillins are 6-acylamino-2,2-dimethyl penam-3-carboxylates.
Penicillins exhibit their bactericidal activity through their ability to interfere with the formation of the bacterial. Penicillins G and V are known as natural penicillins and are marketed in many forms. Their potency is usually expressed as international units.
Pharmacology of penicillin
The pharmacology of penicillins differs markedly from compound to compound. Oral absorption of natural penicillin is poor, as they are acid labile and readily destroyed by gastric acid. Furthermore, the absorption of penicillin is affected by food. Penicillins are also absorbed from skin or mucous surfaces, with sufficient absorption capable of causing allergic reactions.
The penicillins distribute widely throughout the body spaces; nevertheless, the passage into the joints and ocular or cerebrospinal fluid is poor in the absence of inflammation. These agents pass into the bile to varying extents, and can achieve significant levels in the absence of biliary obstruction.
Approximately 30% of the drug is metabolized, with the remaining amount of the drug rapidly excreted through the kidneys by active tubular secretion. Excretion can be competitively inhibited by probenecid, which is a drug used to treat chronic gout and gouty arthritis. In neonates, the elderly, and patients with renal impairment, the half-life of penicillin is significantly lengthened; therefore, the dosage should be modified in order to avoid the risk of neurotoxicity.
References
Further Reading
Last Updated: Aug 22, 2023