Yes, of course. 3D printing can be used to make most things, within certain limitations.
How does 3D printing work? That's a very big question and will depend on which type of 3D printing or additive manufacturing, as it's commonly known, you're referring to.
We would normally divide the additive manufacturing technology into seven different groups. Whilst they all focus on building layer by layer, the way in which those layers are constructed varies according to the different type of additive manufacturing technology that's being used.
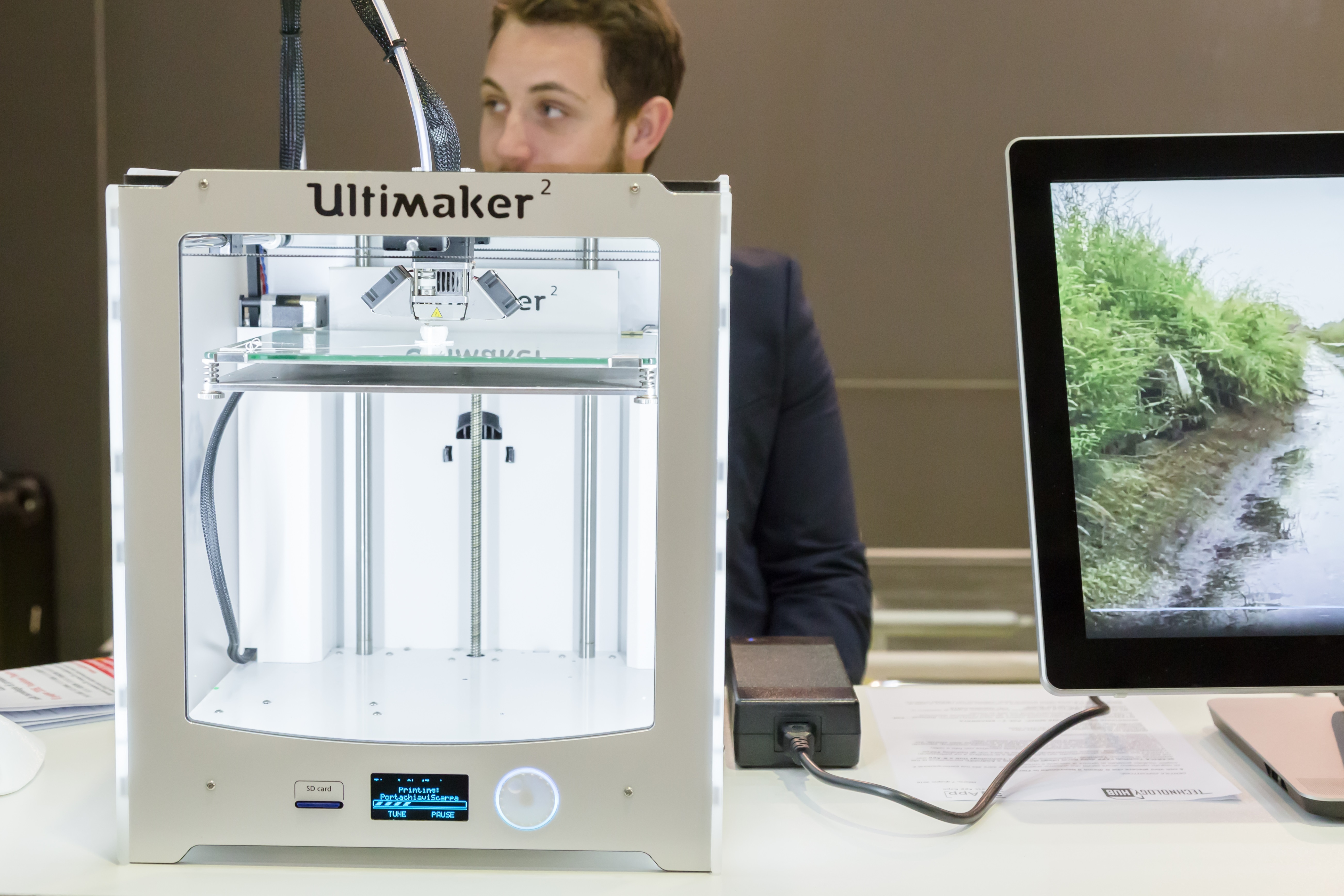
The type that Ultimaker specializes in is called fused filament fabrication. Basically, you have a roll of filaments that is then extruded through a hot end melted and then is bonded layer by layer in increasing layers, to give you the 3D model of the file format you sent across.
Other formats involve lasers; some involve curing using light, different photopolymers and so on, but the most widely adopted form of technology has been fused filament fabrication.
In terms of medical devices, there's been massive growth in this area. Manufacturing or 3D printing has been used in the sector for quite a long time, but there’s been an interesting shift over the last two or three years.
Now, rather than it being outsourced to big bureau printing services who have the in-house expertise to take the DICOM files and convert them into STL files for 3D printing, thanks to the availability of open source software and desktop printers with the accuracy of machines like the Ultimaker, all of a sudden, that’s actually being done by the surgeons, doctors and health practitioners themselves.
© Tinxi / Shutterstock.com
In what other ways has 3D printing been used in medicine so far?
It’s been used in a lot of ways and those ways are growing in number all the time. Right now, 3D printing is being used to create devices to match patient's anatomy, which may be everything from orthopedic and cranial implants, to surgical instruments, dental restorations and external prosthetics.
In terms of the actual areas where it's been used so far, those have been in planning, prosthetics, medical tools, surgical guides, clinical training and patient communication. Patient communication is an often forgotten but very important part of the healthcare process. Then, of course, it's actually helping with diagnosis and we've seen lot of good news stories using the technology as a diagnosis aid.
How does it work in terms of helping with diagnostics?
A great example would be the story that we've got on Ultimaker.com, which is by an orthopedic consultant, Boyd Goldie.
Surgical Planning Using 3D Printed Bones - Ultimaker: 3D Printing Story
Boyd explains how if you're in a trauma situation and you've got a complex fracture, then being able to look at a 3D render of MRI data on a TV screen is very helpful but has limitations.
Experts who've been doing it for many years know which bit of the data to manipulate or how to rotate it to examine it. However, there is no substitute for having said fracture or said bone break actually in your hands, so that you can rotate it and orientate it.
The example on the website is a really badly fractured scapula. What Boyd alludes to is that being able to see that and hold it in his hand means that, not only can he make an assessment of the injury’s severity, but in terms of diagnosis, he can also start to plan exactly what procedure he's going to need to do in order to address the injury.
In the case of this scapula, being able to visualize it and see the realignment that needs to take place, obviously means less of the soft tissue has to be removed from around the area in order to gain access to complete the operation.
Another orthopedic surgeon pointed out to me that this is really powerful because the doctor–patient confidence would go through the roof as the surgical team would be more au fait with exactly what was happening.
However, the really powerful part for me is the removal of less soft tissue from the injury site, because that would mean the bone and the injury would heal more quickly, since the bone would regenerate based on the contact with that soft tissue.
If you think about that on a macro level, people could be a bit smarter by putting a 2000-pound machine alongside the two million-pound MRI scanner, which would not only improve diagnosis, but would also make the actual surgery itself more efficient and help people to heal more quickly.
Then, maybe we wouldn't have the horrible news we hear every day about the bed crisis in the NHS! Boyd's leading the charge on this and proving it can be part of the medical workflow.
© Alexander Tolstykh / Shutterstock.com
How can 3D models impact communication between healthcare professionals and patients?
I think this is one of the real benefits. I studied in the US for a while and one of the biggest determinants of litigation between patients and doctors was whether or not there was good communication and whether or not the doctor took the time to engage on a personal level and explain the circumstances of the injury to the patient.
Obviously, that can be difficult to do, especially when doctors are experts in their disciplines. Most patients aren't medically trained, so it’s a very powerful thing having a tangible model that can explain very visually and also kinesthetically to the patient exactly why they're experiencing the level of pain that they are, why the operation needs to take place and subsequently, what the expected outcome of it is.
Some surgeons have said that some patients actually want to keep it as a souvenir on some occasions, which is quite an unexpected, novel benefit that I had never really considered.
What advances in 3D printing have been key to the medical applications?
There’s been a number. One has been the accuracy and speed of the printers themselves. That's been a huge part of it, because if people are wanting to examine fractures and so on, then obviously you need a certain level of visual accuracy for the people who are going to be using it, whether it be for planning, diagnosis or part of the surgical process.
Another point where there has been a huge breakthrough is in the materials. If we try to gauge the future, we should consider that people are already experimenting with a variety of biomaterials – everything from stem cell research, right the way through to actually trying to print organs. That is a little bit scary in some respects, from a regulation point of view, but it's something that research-wise is being looked at very stringently.
The other area that's made it more accessible has been the software. Back to Boyd's example, if somebody had a serious trauma injury and needed operating on within 24 hours due to the pain levels, then to outsource their DICOM files to a third-party bureau service and have to wait what would typically be seven to ten days before receiving that model back so that you could have all the benefits we just discussed, then, in reality, that's no longer a practical application of the technology.
The operation would need to happen within a much shorter time frame than that. By having a desktop 3D printer as accurate as an Ultimaker, what Boyd does is become master and commander of that workflow, so that he can take the DICOM files from the MRI scanner and convert it using free, open source software, so it's cost-efficient. Then, he can print and have the model within his hands in a matter of hours, rather than a matter of days.
The same concept was also done through a collaboration with Philips. Philips supplies automated hardware and there were all these collaboration opportunities. At one of the recent MRI conferences, we did a collaboration with Philips Healthcare, where Philips were displaying exactly what we were talking about.
They were showing that, “yes, this is the MRI scanner and how we obtain the data,” but they then also had Ultimakers on their stand to display how that digital file was then made tangible for use in 3D printing and how, actually, the work involved was pretty straightforward.
What is Ultimaker’s vision?
For Ultimaker, it all started back in 2011 where they were trying to make 3D printers accessible to as many people as possible. The RepRap project was designed to make 3D printers that can replicate themselves. Then, Ultimaker took that open source, collaborative ethos and wanted to apply it to a printer that was more robust and reliable, so that actually, the frustration about using the printer itself was removed.
Therefore, it became about what you were producing rather than the printing process in its own right. Fast forward to 2017, and we're very proud to say that we're the market leaders in Europe now and we've done that through remaining open, looking to collaborate and, most importantly, making sure that we focus on user experience and create local feedback loops.
That means people can constantly look to improve, not only the hardware we are offering, but also they can tell us what they need in their individual applications.
How does the Ultimaker 3 differ from previous models?
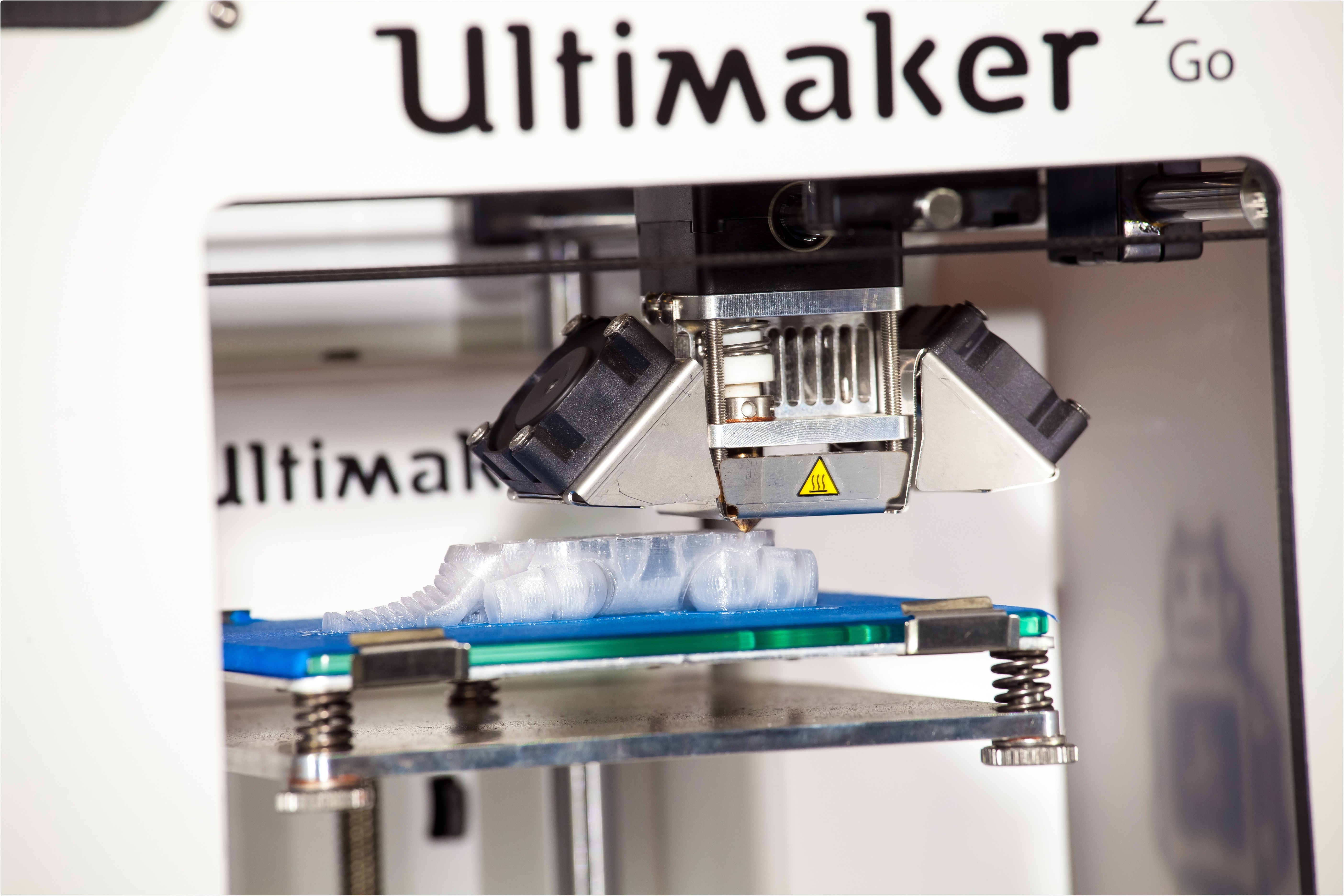
The Ultimaker 3 has been a game-changer in many ways. Part of the reason that we were so excited about launching it last year was the fact that it has dual extrusion. Now, people who aren’t au fait with 3D printing could say that might seem like a very technical term, but in layman's terms, it means that instead of just having one material being printed you can now print in two different materials.
That offers visualization benefits. For example, one could print in red and then a different color in order to highlight an artery in a particular model. However, what's actually potentially more exciting moving forwards, is that some of the complexities that are inherent to the physical structures within the body would have been very difficult to print with a single extrusion.
Previously, you wouldn't have been able to get the necessary support structures into the model, so that the model was accurate and representative of real life. By having a second material that can be extruded through the printer, we can actually put a soluble support material in there.
Rather than having a messy, post-process procedure where some of the plastic has to be removed in order to see that fracture in the bone, you can now place it into a water bath or underneath a tap.
It's completely green and very biodegradable, meaning you could actually wash away the support structure, leaving you with only the intended model at the end of the process. What that means in real terms is that the complexity is no longer restricted by the material and can be printed through an Ultimaker3.
Do you think it will be possible to print in multiple different materials in the future?
Absolutely and it's something people are looking at. One of the big challenges with that is obviously the chemistry involved in creating the right environments for the materials to be printed in.
As is the way in any form of technology and also in life, the more variables there are, the harder it is to deliver a reliable result. Back to your point about the Ultimaker vision, it's always been about bringing to market stuff that works, rather than something that might have potential.
I think there will be 3D printing solutions in the future at this price point, which are generally multi-material, rather than just dual material. Right now, if you go for one of the more top-end, high-level industrial machines that cost hundreds of thousands of pounds, you can already print in multicolor and in multi-material, but obviously the capital outlay involved in getting access to some of these machines can be problematic.
What we're finding with the Ultimaker is that, because the price point of the machine is what it is and also the cost of the filaments and the software moving forwards is pretty low, then more and more people are building confidence in this machine and reaping the benefits.
What do you think the future holds for 3D printing in medicine?
There's already some exciting stuff going on, in terms of people actually looking to produce body parts and so on. I think an example of where the short-term future lies is a fantastic project called The Open Bionics. The people involved basically print external prosthetics using Ultimakers, which then incorporates a series of sentences that attach to the patient's arm.
Instead of having to pay thousands and thousands of pounds for a smart prosthetic, all of a sudden, thanks to 3D printing, people will be able to get access to this sort of technology at a much lower price.
What's really interesting about the Open Bionics project, is that Disney saw the application of it, and was so excited about it, that they actually licensed some of their intellectual property to Open Bionics. So, we can now have a prosthetic Frozen arm, for example, or prosthetic Iron Man hand.
In terms of some of the stigma kids would have to live with as a consequence of growing up with not having all their limbs, as would be standard in a playground, now, suddenly, they can have Elsa's arm or Tony Stark's arm or something like that. It's no longer a stigma and is suddenly a status symbol.
Looking a little bit further than that, I think there will be mass adoption. I think that once people start to put a 2000-pound machine alongside a two million-pound machine, which would suddenly increase the value of the machine’s output, each case of this will start to resonate and we'll start to see them in orthopedic divisions of hospitals up and down the country.
If we look at some of the exciting research that's going on at the moment, the delivery method on 3D printing allows people to have bespoke medication, so instead the off-the-shelf drugs we take, which are very much one, three or four sizes fits all, now you'll be able to have medication that is blended according to individual patient’s requirements.
If you think we could be producing body parts and also the right dosage of medication, then these could become really powerful tools that are in every health practitioner's toolset, if you will.
Another case that might be interesting to look at is the program we're supporting in the US at Jefferson University. It is called the JeffDESIGN Program and what they are basically doing is making sure that any medical students coming through the medical training programs there are getting access to this technology and being encouraged to be innovative in terms of the way they will provide healthcare.
I think if we stargaze a little bit, then giving these medical practices technology to solve problems in a way that's not previously been done before, will open up a whole world of possibilities, which is really exciting.
Do you think 3D printing will impact healthcare in any other ways?
One point is the power of these tools to be used to educate the next generation of healthcare practitioners. When I was growing up at school, we were allowed to dissect things in the classroom and I know that health and safety restrictions, certainly in the UK, have changed that, which is not necessarily for the better.
If I'm going to be having an operation in 15 years' time, I would much prefer the person doing the operation to have been performing trial and error-based studies with anatomically correct 3D printed parts, if they couldn't actually get their hands on the real thing.
Another potential impact is in mental health. I can see a mental health time bomb ticking away in the UK. We've got first-hand examples of people who've been struggling, shall we say, with some various forms of mental health issues, who find 3D printing really empowering, because it gives you that intrinsic gratification of having made and completed something, which is very difficult to achieve in normal walks of life.
There is no academic or empirical evidence of this yet, but I think that, over the coming years, we'll hear about more and more cases where people who have various afflictions have been able to turn the corner, thanks to the power of 3D printing. I think it could be a powerful tool for addressing some of the challenges we’ve been having in society.
I have almost the perfect first-hand example. One of our technical support employees is somebody that I've known for many, many years. He's suffered with anxiety and a form of depression for many years. Having tried absolutely everything such as various forms of counseling, and support from friends and family as much as possible, he'd still not been able to make the breakthrough.
We gave him an Ultimaker Original kit to assemble from scratch, which obviously involves technical skills and certain engineering principles and so on. By the end of the building process, he was confident enough to start conversing with strangers again, which is really difficult to do when you've been in that place.
I'm now proud to say that two years later, he's leading the charge as part of our technical support team. Considering he’s been out of the game, so to speak, for many years due to his anxiety and depression, to now see him back leading events for us is really powerful.
One project we support and are part of is the Blair Project in the Wigan area. There, people work with pre-NEAT children, some of whom have mental health challenges or learning difficulties. I've heard on numerous occasions from head teachers, about pupils who refuse to engage in the classroom who have been given access to 3D printers and instead of using profanity to address the teachers, they are now asking teachers inquisitive questions.
I think if we can get this message out, then we can not only solve some of the existing issues that are bubbling away, but also potentially stop people falling into some of the traditional traps.
Where can readers find more information?
About Paul Croft
Paul is a Director of UltimakerGB the UK & Ire operations for Ultimaker and the founder of the CREATE Education Project.
The CREATE Education Project was launched in 2014 and we are excited about sharing 3d printing and associated technologies with everyone.
Twitter
@UltimakerGB @UltimakerCREATE @Ultimaker