2. What should I know before I use LONSURF?
Do not use if you have ever had an allergic reaction to LONSURF or any of the ingredients
listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines,
or are pregnant or plan to become pregnant or are breastfeeding.
3. What if I am taking other medicines?
4. How do I use LONSURF?
Your doctor will usually prescribe LONSURF for 10 days during the first two weeks
and then stop for two weeks.
This two week on, two weeks off treatment period is one 'cycle' of treatment.
You will then begin another treatment cycle following the above pattern.
The specific dosing schedule is outlined in the full CMI.
5. What should I know while using LONSURF?
|
Things you should do
|
Remind any doctor, dentist, nurse or pharmacist you visit that you are using LONSURF.
Tell your doctor immediately if you become pregnant during treatment with LONSURF,
or plan to become pregnant.
Tell your doctor if you are breast-feeding while being treated with LONSURF.
If you are about to have any blood tests, tell your doctor that you are taking this
medicine. It may interfere with the results of some tests.
|
|
Things you should not do
|
Do not take LONSURF to treat any other complaints unless your doctor tells you to.
Do not stop taking LONSURF, or lower the dosage, even if you are feeling better, without
checking with your doctor.
|
|
Driving or using machines
|
Do not drive or operate machinery until you know how LONSURF affects you. Speak with
your doctor about when you can resume these activities.
|
|
Looking after your medicine
|
Store in a cool dry place away from moisture, heat and sunlight. Keep out of reach
of children.
Keep your tablets in the pack until it is time to take them.
|
6. Are there any side effects?
Tell your doctor, nurse or pharmacist as soon as possible if you do not feel well
while you are taking LONSURF. All medicines can have side effects. Sometimes they
are serious, most of the time they are not.
If you experience neutropenia, anaemia, vomiting and diarrhoea, thrombocytopenia,
febrile neutropenia or abdominal pain after taking LONSURF, please seek urgent medical attention.
Active ingredient(s):
trifluridine and tipiracil
Full Consumer Medicine Information (CMI)
This leaflet provides important information about using LONSURF. You should also speak to your doctor or pharmacist if you would like further information
or if you have any concerns or questions about using LONSURF.
Where to find information in this leaflet:
1. Why am I using LONSURF?
LONSURF contains the active substances trifluridine and tipiracil.
• Trifluridine stops the growth of cancer cells.
• Tipiracil stops the trifluridine from being broken down by the body, helping trifluridine
to work longer.
LONSURF is used to treat cancer by slowing down the growth and spread of cancer cells.
LONSURF is a type of cancer chemotherapy which belongs to a group of medicines called
'cytostatic antimetabolite medicines'.
LONSURF is used to treat adults with colon or rectal cancer - sometimes called 'colorectal'
cancer. It is also used to treat gastric cancer- sometimes called 'stomach' cancer.
It is used when the cancer has spread to other parts of the body.
It is used when other treatments have not worked - or when other treatments are not
suitable for you.
2. What should I know before I use LONSURF?
Warnings
Do not use LONSURF if:
you are allergic to tipiracil and/or trifluridine, or any of the ingredients listed
at the end of this leaflet.
Always check the ingredients to make sure you can use this medicine.
Do not take LONSURF after the expiry date printed on the pack.
Do not take LONSURF if the packaging is torn or shows signs of tampering.
Check with your doctor if you:
have any other medical conditions especially the following:
kidney problems
LONSURF is not recommended in some patients with kidney problems. Before you start
each treatment cycle of LONSURF, your doctor will perform blood tests to monitor your
kidneys to see how they are working.
liver problems.
LONSURF is not recommended in some patients with liver problems. Before you start
each treatment cycle of LONSURF, your doctor will perform blood tests to monitor your
liver to see how your liver is working. Treatment with LONSURF may lead to a higher
risk of liver problems.
take any medicines for any other condition.
LONSURF contains lactose.
If you have been told by your doctor that you have an intolerance to some sugars,
contact your doctor before taking this medicine.
During treatment, you may be at risk of developing certain side effects. It is important
you understand these risks and how to monitor for them. See additional information
under Section
6. Are there any side effects?
Pregnancy and breastfeeding
It is important to tell your doctor if you are pregnant or intend to become pregnant,
or if you are breastfeeding or intend to breastfeed.
Pregnancy
Do not take this medicine if you are pregnant or think you might be pregnant.
Tell your doctor if you are pregnant or intend to become pregnant.
Like most anti-cancer medicines, LONSURF is not recommended for use during pregnancy.
However, if you need to take LONSURF during your pregnancy, your doctor will discuss
with you the benefits and risks of taking it.
You must not become pregnant while taking LONSURF, as this medicine may harm your
unborn baby.
Contraception
You and your partner should use effective methods of contraception while taking this
medicine. You should also do this for 6 months after you stop taking the medicine.
If you or your partner becomes pregnant during this time, you must talk to your doctor
or pharmacist straight away.
Breastfeeding
Do not breast-feed while taking LONSURF.
Tell your doctor if you are breast-feeding or planning to breast-feed. This medicine
may interfere with the growth and development of your baby.
Fertility
LONSURF may reduce fertility in both men and women. Your doctor will advise you of
your options prior to starting treatment.
Children and adolescents
LONSURF is not recommended for use in children and adolescents. Safety and effectiveness
have not been established in this age group.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any
medicines, vitamins or supplements that you buy without a prescription from your pharmacy,
supermarket or health food shop.
LONSURF and other medicines may interact. These include medicines used for treatment
of HIV, such as zidovudine. Zidovudine may not work as well if you are taking LONSURF.
You may need different amounts of your medicine, or you may need to take different
medicines. Your doctor will advise you.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins
or supplements you are taking and if these affect LONSURF.
4. How do I use LONSURF?
Always take LONSURF exactly as your doctor has told you to.
Follow all directions given to you by your doctor or pharmacist carefully. They may
differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist
for help.
MyLonsurf Dosing Calendar
The MyLonsurf dosing calendar has been created to help you understand your dose and
treatment cycle. The MyLonsurf dosing calendar also contains important information
on how many tablets of each strength you need to take for your current four week cycle.
Ask your doctor if you have not received, or have misplaced, your MyLonsurf dosing
calendar.
How much to take / use
Your doctor or pharmacist will tell you how many tablets you will need to take each
time. The dose depends on your weight and height and if you have kidney problems.
LONSURF comes in two strengths. Your doctor may prescribe both strengths for your
prescribed dose.
You will take the dose two times a day - half the dose in the morning and half the
dose at night.
Swallow LONSURF tablets whole, with a glass of water.
Wash your hands after handling LONSURF tablets.
When to take / use LONSURF
Your doctor will usually prescribe LONSURF for 10 days during the first two weeks
and then stop for two weeks. This two week on, two weeks off treatment period is one
'cycle' of treatment.
The specific dosing schedule is as follows:
Week 1 - take the dose two times a day for five days. Then have two days off - no
medicine.
Week 2 - take the dose two times a day for five days. Then have two days off - no
medicine.
Week 3 - no medicine.
Week 4 - no medicine.
You will then begin another treatment cycle following the above pattern.
Take LONSURF immediately after your morning and evening meals, or within one hour
after completion of your morning and evening meals.
How long to take it
Your doctor will continue to treat you with LONSURF as long as you are receiving benefit
from therapy. Your doctor may need to reduce your dose or may decide to stop treatment
if you experience serious side effects.
Do not stop taking it unless your doctor tells you to - even if you feel better.
If you do not understand the instructions provided, ask your doctor or pharmacist
for help.
If you forget to use LONSURF
If you miss a dose, do not take the missed dose at a later date. Make a record of
the dose you missed and tell your doctor and/or pharmacist immediately.
Do not take a double dose to make up for the dose you missed.
This may increase the chance of you getting an unwanted side effect.
If you have trouble remembering to take your medicine, ask your pharmacist for some
hints.
If you use too much LONSURF
If you think that you have used too much LONSURF, you may need urgent medical attention.
You should immediately do one of the following:
phone the Poisons Information Centre
(by calling
13 11 26), or
contact your doctor, or
go to the Emergency Department at your nearest hospital.
You should do one of the above even if there are no signs of discomfort or poisoning.
5. What should I know while using LONSURF?
Things you should do
Tell any other doctors, dentists, and pharmacists who are treating you that you are
taking LONSURF.
If you are about to be started on any new medicines, tell your doctor, dentist or
pharmacist that you are taking LONSURF.
Tell your doctor immediately if you become pregnant during treatment with LONSURF,
or plan to become pregnant.
Tell your doctor if you are breast-feeding while being treated with LONSURF.
If you are about to have any blood tests, tell your doctor that you are taking this
medicine. It may interfere with the results of some tests.
Things you should not do
Do not give LONSURF to anyone else, even if their symptoms seem similar or they have
the same condition as you.
Do not take LONSURF to treat any other complaints unless your doctor tells you to.
Do not stop taking LONSURF, or lower the dosage, even if you are feeling better, without
checking with your doctor.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how LONSURF
affects you.
Looking after your medicine
Keep your tablets in the pack until it is time to take them.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do
not store it:
in the bathroom or near a sink, or
in the car or on window sills.
Keep it where young children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place
to store medicines.
When to discard your medicine
Do not take LONSURF after the expiry date printed on the pack.
The expiry date is printed on the carton and bottle after "EXP" (e.g. 11 17 refers
to November 2017). The expiry date refers to the last day of that month.
Do not take LONSURF if the packaging is torn or shows signs of tampering.
If it has expired or is damaged, return it to your pharmacist for disposal.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy
for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of
them are minor and temporary. Sometimes they are serious, most of the time they are
not. However, some side effects may need medical attention. You may need medical treatment
if you get any of the side effects listed below, after taking LONSURF alone or in
combination with another type of cancer chemotherapy, bevacizumab.
See the information below and, if you need to, ask your doctor or pharmacist if you
have any further questions about side effects.
Serious side effects
|
Serious side effects
|
What to do
|
|
Skin
sudden signs of allergy such as skin rash, itching or hives, swelling of the face,
lips, tongue or other parts of the body
Gastrointestinal
vomiting and diarrhoea, which may lead to a dehydration if severe or persistent.
abdominal pain. The signs include intense stomach or abdominal pain that can be associated
with vomiting, blocked or partly blocked bowel, fever or swelling of the abdomen.
severe gastrointestinal problems: ascites, colitis, acute pancreatitis, ileus and
subileus. The signs include intense stomach or abdominal pain that can be associated
with vomiting, blocked or partly blocked bowel, fever or swelling of the abdomen.
Respiratory and heart
shortness of breath, wheezing or difficulty breathing
pulmonary embolism - blood clots in lungs. The signs include shortness of breath and
pain in the chest or in the legs.
Blood and investigations
neutropenia – a decreased number of white blood cells. The signs include chills, fever
(febrile neutropenia), sweating or other sign of infection.
anaemia - a condition in which there is a decreased number of red blood cells. The
signs include feeling short of breath, tiredness or looking pale.
thrombocytopenia - low blood platelet count. The signs include unusual bruising or
bleeding.
Infections
septic shock. The signs include chills, fever, sweating or other sign of infection
|
Call your doctor straight away, or go straight to the Emergency Department at your
nearest hospital if you notice any of these serious side effects.
|
Less serious side effects
|
Less serious side effects
|
What to do
|
|
Skin and hair
rash, itchy or flaky skin
skin flushing
dry skin
raised itchy rash, hives, acne
sweating more than normal and, nail problem
raised red skin, blisters, skin sloughing off
swelling of mucous membranes - this could be inside the nose, throat, eyes, vagina,
lungs or gut
sensitivity to light
hair loss
Gastrointestinal
decreased appetite
nausea - feeling sick
constipation
weight loss
bloating, passing gas, indigestion
inflammation in lower part of digestive tract
swelling or bleeding in your bowel
inflammation or increased acid in your stomach or gullet, reflux
inflammation and infection in your gut
inflammation in upper part of digestive tract
pain in upper or lower part of digestive tract
inflammation or bleeding in your bowel
increase in the diameter of the bile duct
Mouth and throat
changes in taste
swelling of mucous membranes in mouth
mouth pain or problems
mouth ulcers
painful tongue, retching
bad breath, tooth decay, tooth problems, gum infections
sore throat, hoarse voice, problems with your voice
bad breath, gum problems, bleeding gums
polyps inside your mouth
Kidney and liver related
increased bilirubin in your blood - can cause yellowing of skin or eyes
increased liver enzymes
protein in your urine
liver disorder
inflammation or infection of bile ducts. The signs may include pain on the right side
of your stomach.
kidney failure. The signs include little or no urine, drowsiness, nausea, vomiting,
breathlessness
blood in urine
urine retention - problems passing water, incontinence - loss of bladder control
inflammation in your bladder
changes in urine test
Respiratory and heart
Interstitial lung disease has been reported in patients receiving the medicine in
Japan. The signs include difficulty in breathing, shortness of breath, with cough
or fever.
cough, feeling short of breath, infection of the sinuses, throat, airway or lungs,
chest infections
more noticeable heart-beat, chest pain
abnormal increase or decrease in heart rate
accumulation of fluid in the lungs
changes in your heart trace (ECG - electrocardiogram)
Blood and investigations
reduced white blood cells called leucocytes - can increase your risk for infection
low levels of albumin or total protein in the blood
reduced number of white blood cells called lymphocytes - can increase your risk for
infection
blood test results indicating problems with clotting making you bleed more easily
increased number of white blood cells called monocytes
increased lactate dehydrogenase level in your blood
low levels of phosphates, sodium, potassium or calcium in your blood
reduced white blood cells called monocytes - can increase your risk for infection
hyperglycaemia - high blood sugar, urea, creatinine and potassium in your blood
blood test result indicating inflammation (C-Reactive Protein increased)
reduced white blood cells called granulocytes - can increase your risk of infection
increased salt in your blood
blood clots, e.g. in the brain or legs
low level of total protein in the blood
Infections
viral infection
shingles - pain and vesicular rash on skin over nerve tracts affected by nerve inflammation
from herpes zoster virus
infections: bacterial or fungal
infection in your bladder
athlete’s foot - fungal infection of feet, yeast infections
Musculoskeletal
swelling in your hands or legs or feet
pain in your joints
muscle pain
swelling or pain in your joints or big toes
pain in your arms or legs
pain, including pain from the cancer
bone pain, muscle weakness or spasms,
feeling of numbness or pins and needles in hands or feet
redness, swelling, pain on the palms of your hands and soles of your feet (hand-foot
syndrome)
Nervous system
feeling dizzy, headache
low or high blood pressure
vertigo - feeling of spinning
anxiety
problem with sleeping or falling asleep
non-severe neurological troubles
feeling lethargic or tired
feeling dizzy, headache
burning sensation, unpleasant, increased or loss of sense of touch
fainting (syncope)
Eye, ear and nose
redness, itching of the eye, eye infections, watery eyes
vision troubles as blurred vision, double vision, decreased vision, cataracts
dry eyes
ear pain
runny or bloody nose, sinus problems
Reproductive system
changes in the menstrual cycle
General
dehydration
fever
fatigue - feeling very tired
malaise - feeling generally out of sorts
general feeling of discomfort
feeling of being cold
|
Speak to your doctor if you have any of these less serious side effects and they worry
you.
|
Tell your doctor or pharmacist if you notice anything else
that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can
report side effects to the Therapeutic Goods Administration online at
www.tga.gov.au/reporting-problems . By reporting side effects, you can help provide more information on the safety of
this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop
taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What LONSURF contains
|
Active ingredients
(main ingredients)
|
Trifluridine
Tipiracil (as hydrochloride)
|
|
Other ingredients
(inactive ingredients)
|
Lactose monohydrate
Pre-gelatinised starch
Stearic acid
Hypromellose
Macrogol (8000)
Titanium dioxide (E171) Magnesium stearate
The printing ink contains: Shellac
Iron oxide red (E172)
Iron oxide yellow (E172), Titanium dioxide (E171)
Indigo carmine aluminium lake (E132)
Carnauba wax
Talc
|
|
Potential allergens
|
Lactose
|
Do not take this medicine if you are allergic to any of these ingredients.
What LONSURF looks like
LONSURF 15/ 6.14 is a white, biconvex, round, film-coated tablet, printed with "15"
on one side and "102" and "15 mg" on the other side in grey ink.
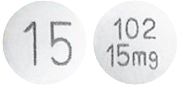
(Tablet image not actual size)
LONSURF 20 /8.19 is a pale red, biconvex, round, film-coated tablet, printed with
"20" on one side and "102" and "20 mg" on the other side in grey ink.
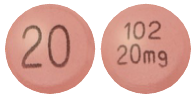
(Tablet image not actual size)
Each pack contains 20 film-coated tablets (2 blisters of 10 tablets each) or 60 film-coated
tablets (6 blisters of 10 tablets each).
(AUST R 273239: LONSURF 15/6.14 tablets
AUST R 273238: LONSURF 20/8.19 tablets).
Who distributes LONSURF
Servier Laboratories (Aust.) Pty. Ltd.
Level 4, Building 9
588A Swan Street
Burnley, 3121, Victoria
This leaflet was prepared in November 2024.