Breast cancer is characterized by the growth of abnormal cells in the breast. It can occur in the lobules, or milk-producing glands of the breast, the ducts that carry milk to the nipple, or the connective tissue of the breast.
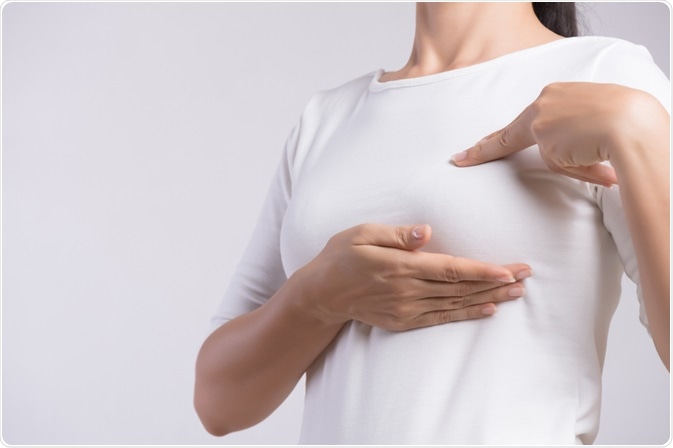
Woman checking her breasts for lumps. Image Credit: siam.pukkato/Shutterstock.com
The most common forms of breast cancer are invasive lobular carcinoma, whereby cancer cells develop in the lobules and spread into the surrounding tissue, and invasive ductal carcinoma, where cancer cells grow outside of the ducts into other parts of the breast tissue.
Breast cancer is the commonest form of cancer and the leading cause of cancer death among women, affecting about one in eight women during their lifetime. Globally, over 2.2 million women were diagnosed with breast cancer and approximately 685,000 died from breast cancer in 2020. The incidence of breast cancer has risen significantly since the 1970s. When population growth is taken into account, rates have increased four-fold.
Early detection
Breast cancer is staged from 0 to IV and relates to the degree to which the cancer has advanced. In stages 0 and I, the cancer is located only in the breast. At stage II, the cancer has either grown or spread to the surrounding lymph nodes. At stage III it has advanced and spread to surrounding tissues, and at stage IV the cancer is metastatic, and the most common sites are in the brain, bones, and liver.
The stage at which the cancer is diagnosed and treated has dramatic ramifications for the 5-year survival rate. If identified at either stage 0 or 1, the 5-year survival rate is 99%. If identified at stage II, the survival rate is 86%, falling to 28% if identified at stages 3 or 4.
Early identification of breast cancer is critical for favorable clinical outcomes. Most healthcare systems, however, only offer breast screening using mammograms to women aged fifty and above. This is due to the risk of developing cancer increasing with age, and the risks involved with exposure to radiation during an x-ray. As research has shown that many breast cancers are first detected by patients, self-examination can be a useful method of identifying breast changes at the earliest possibility.
A guide to self-examination
Regular self-examination, when paired with other screening methods can be a useful tool to identify cancer early. It is convenient, no-cost, and can be completed at women’s convenience in their own homes.
Step 1: Stand directly in front of a mirror, keeping the shoulders straight and hands-on-hips. Begin with a thorough visual examination, checking whether breasts are their usual size, shape, and color, and evenly shaped without visible distortion.
Step 2: Raise the arms above the head and check for the changes as per stage 1.
Step 3: Check for signs of discharge from the nipple. This can be watery, yellowish, or bloody.
Step 4: Lying down and keeping the fingers flat and together, feel across the entire breast using a circular motion. This should extend from the collarbone to the top of the abdomen, and from the armpit to the cleavage. Using the left hand to feel the right breast, and vice versa, follow a pattern to ensure the entire breast area is covered.
Step 5: Repeat the process in step 4 when standing or sitting.
Self-examination of the breasts should be completed once a month to become familiar with how the breasts normally look and feel. It may be useful to keep a journal to record the findings of examinations to help identify changes. Changes that should be reported to a doctor include:
- Any change to the size, shape, or outline of the breasts.
- Any change to the appearance or texture of breast tissue, such as dimpling or puckering.
- Any new lump or thickening in one breast or armpit.
- Nipple discharge that is not milky, such as yellow or bloody fluid.
- Any change in nipple position, including nipple inversion or pointing in a new direction.
- Any breast discomfort or pain that is novel and persistent.
Effectiveness of self-examination
Studies that have evaluated the impact of breast self-examination have compared tumor characteristics between women who practice self-examination and those who do not and have demonstrated that self-examination is associated with reduced overall tumor size and the likelihood of cancer spread to the lymph nodes. Those who self-examine are also more likely to seek medical care more rapidly. The benefits of self-examination are particularly favorable when women receive specific education regarding self-examination techniques.
References
- Baxter, N., & Canadian Task Force on Preventive Health Care (2001). Preventive health care, 2001 update: should women be routinely taught breast self-examination to screen for breast cancer?. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 164(13), 1837–1846.
- Foster, R. S., Jr, Lang, S. P., Costanza, M. C., Worden, J. K., Haines, C. R., & Yates, J. W. (1978). Breast self-examination practices and breast cancer stage. The New England journal of medicine, 299(6), 265–270. https://doi.org/10.1056/NEJM197808102990601
- Kashgari, R. H., & Ibrahim, A. M. (1996). Breast cancer: attitude, knowledge, and practice of breast self-examination of 157 Saudi women. Journal of family & community medicine, 3(1), 10–13.
- Koriech O. M. (1996). Breast cancer and early detection. Journal of family & community medicine, 3(1), 7–9.
- Schneider, A. P., 2nd, Zainer, C. M., Kubat, C. K., Mullen, N. K., & Windisch, A. K. (2014). The breast cancer epidemic: 10 facts. The Linacre Quarterly, 81(3), 244–277. https://doi.org/10.1179/2050854914Y.0000000027
- https://www.breastcancer.org/symptoms/testing/types/self_exam
Further Reading
Last Updated: Jan 17, 2022