Introduction
What Are Sex Hormones?
How Are Sex Hormones Produced?
The Physiological Effect of Sex Hormones
Estrogen
Progestrogens: Progesterone
Androgens
References
Sex hormones are considered critical regulators of sex-related characteristics in both males and females during puberty. They also play a critical role in regulating skeletal growth during periods of increasing and decreasing skeletal mass. Outside of this endocrine and musculoskeletal function, they influence a broad spectrum of normal and abnormal neurological function and immune function.
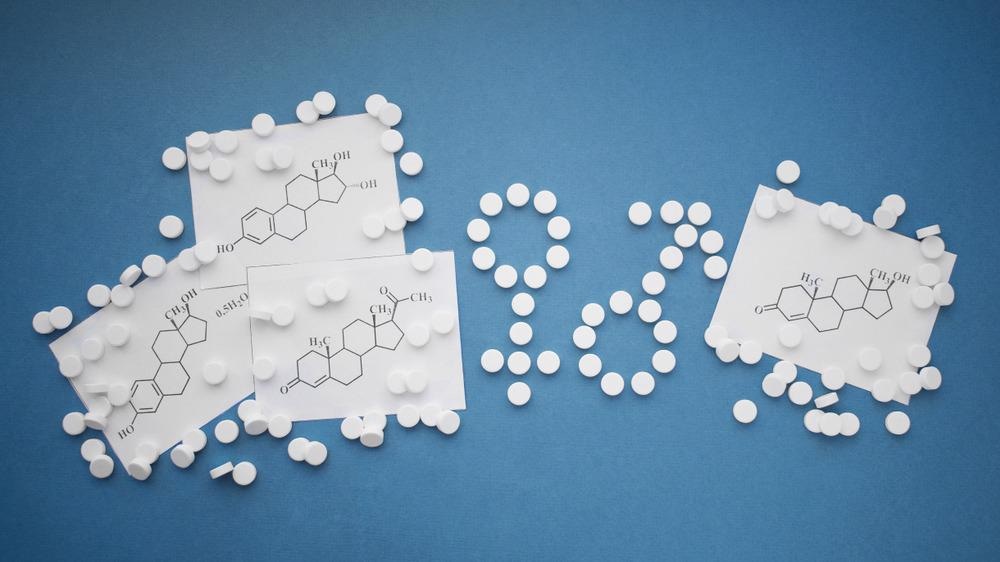
Image Credit: linda_kar/Shutterstock.com
What Are Sex Hormones?
Sex hormones are also known as sex steroids, gonadal steroids, and gonadocorticoids. These are steroid-based hormones that interact with vertebrate steroid hormone receptors.
Sex hormones principally exert their effects to produce sexual differentiation and reproduction. In females, the ovary produces three classes of sex steroids. These include estrogens, progestins, and androgens.
The effects of these three sacks hormones are mediated by slow rate genomic mechanisms acting through nuclear receptors and non-genomic mechanisms through membrane-associated receptors to elicit several signaling cascades in a fast response.
The polypeptide hormones luteinizing hormone, follicle-stimulating hormone, and gonadotrophin-releasing hormone are associated with the sex hormones and can produce sex-regulated responses but are not regarded as sex hormones themselves.
How Are Sex Hormones Produced?
The gonads produce sex hormones, that is, the ovaries or the testes alongside the adrenal glands. Alternatively, they are produced due to the biochemical conversion of other steroids present in the liver or adipose tissue.
The Physiological Effect of Sex Hormones
Generally speaking, sex hormones play an essential role in reproduction and sexual development. The following functions are elicited from the sex hormones: Reproduction and sexual development, puberty, cholesterol regulation, high growth, distribution of body fat, and inflammatory response. The concentrations of these hormones vary throughout an individual's lifetime and are influenced by several factors, including age, menstruation, menopause, stress, medication, and recreational drug use.
The activity of steroid hormones is carried out by receptors belonging to the family of nuclear substances. As stated, sex hormones act through both genomic and non-genomic mechanisms of action and result in the transduction of signals.
Estrogen
Estrogen is found in the blood and interstitial fluid. As a result of binding, estrogen penetrates the cell membrane, entering the cell nucleus and binding to its receptor. The hormone-receptor structure that results produces a dimer stop binds to a specific sequence in the genome called the estrogen-response elements (EREs) in areas of the genome that control different gene regulation of transcription.
Estrogen act through several nuclear receptors and affects the endometrial, vaginal, and breast tissues.
Estrogen's non-genomic activities include removing granular calcium cells and mediating uterine blood flow. Non-genomic activity occurs in the absence of cellular receptors.
Estrogens antagonize the effects of the parathyroid hormone, minimizing the loss of calcium from bones and thus helping to keep bones strong. Estrogens are used as hormone-replacement therapy (menopause), oncology, and contraceptives.
Overall, estrogens act to develop and maintain internal and external genitalia (i.e., the fallopian tubes, uterus, vagina, vulva, clitoris, etc.), the appearance and functionality of the skin by increasing vascularization; develop soft, textured, and smooth skin; increase osteoblastic activity to improve bone density; the retention of sodium, chloride, and water by the kidney; and lower the amount of cholesterol in the body.

Image Credit: GoodIdeas/Shutterstock.com
Progestrogens: Progesterone
The corpus luteum and the placenta secrete progesterone. It plays an essential role in the menstrual cycle and pregnancy. It is also used in hormonal contraception as well as long-term ovarian suppression in other medical conditions such as dysmenorrhea, endometriosis, hirsutism, and other bleeding disorders. It is often combined with other sex hormones such as estrogen to reduce the risk of uterine or cervical cancer. Like estrogen, progesterone is vital in hormone replacement therapy and feminizing hormone therapy.
Progesterone elicits a variety of essential functions in the body. It is also considered a crucial metabolic intermediate along the production pathways for other endogenous steroids, which include not only the sex hormones but also corticosteroids and neurosteroids.
The effects of progesterone are amplified in the presence of estrogen. Estrogens act through their estrogen receptors to upregulate or induce the extraction of the progesterone receptor. Too much progesterone results in the compromised activity of the hormone aldosterone, which reduces sodium retention, resulting in natriuresis and a reduction in the volume of extracellular fluid. Too little progesterone is conversely associated with sodium retention and subsequent increase in extracellular fluid volume.
Progesterone acts in the reproductive system via non-genomic signaling to act on sperm. The effects of progesterone on sperm include changes and intracellular calcium signaling, which is thought to be related to the regulation of sperm motility.
Progesterone is principally involved in pregnancy and has many functions concerning the development of the fetus. These include altering the endometrium to be prepared for implantation, thickening the vaginal epithelium and cervical mucus to make it impenetrable to sperm, and producing an anti-mitogenic effect in the endometrial epithelial cells. Progesterone also inhibits lactation during pregnancy.
In the absence of pregnancy, progesterone typically decreases, which facilitates menstruation; menstruation is considered a consequence of progesterone withdrawal.
Outside of the reproductive system, progesterone is implicated in developing the breasts in conjunction with prolactin. It is also implicated in the pathophysiology of breast cancer. Like estrogen, progesterone is also involved in skin health.
During menopause, decreased levels of the female sex hormones result in atrophy, thinning, increased skin wrinkling, and an overall reduction in skin elasticity, strength, and firmness. Concomitantly, hormone replacement therapy which includes progesterone alone or in combination with estrogen results in increased collagen content, thickness, elasticity, hydration, and concentration of surface lipids.
The application of estrogen topically has also been found to produce beneficial effects; for example, topical application of 2% progesterone has been shown to significantly increase skin elasticity and firmness as well as produce observable decreases in wrinkles. Overall, like estrogen, progesterone can be protective against skin aging.
Interestingly, progesterone is implicated in the brain and may play a role in addiction. Progesterone enhances the function of the serotonin receptors; that imbalance in progesterone has the potential to result in significant neurochemical issues. An insufficient amount of progesterone can result in behaviors designed to enhance serotonin activity, such as alcohol, cannabis, and nicotine.
Androgens
Androgens are the principal sex determinant steroid in males. However, both males and females produce androgens. Males with too little androgens typically have a low sex drive and suffer from gynecomastia. Conversely, females with excessive androgen expression may develop hirsutism, acne, and other issues.
Testosterone is the most common under and is produced by the ovaries and the testicles.
In all genders, the androgens play a role in bone density, muscular development, onset and maturation during puberty, the production of red blood cells, libido, and sexual function. In men, androgens elicit a differential effect. These include deepening the voice through vocal cord lengthening, hair growth, particularly on the face, scalp, underarms, chest, and genitals, and the development of sperm.
In women, androgens regulate menstruation, prevent osteoporosis through the minimization of bone loss, aid in conception on pregnancy, and stimulate the growth of pubic and underarm hair.
Sex hormones play essential roles in both males and females regarding sexual development and function; each illicit its unique effects. To this end, androgens are considered male sex hormones as they produce masculinizing effects, while estrogens and progestogens are considered female hormones. However, all sex hormones are present in each gender, where both are implicated in a range of organs and systems.
References:
- Hyman M. Schipper. Chapter 22 - Sex Hormones and the Nervous System. Editor(s): Michael J. Aminoff, Neurology and General Medicine (Fourth Edition). Churchill Livingstone. 2008, Pages 409-426. https://doi.org/10.1016/B978-044306707-5.50025-0.
- Guerriero G. (2009) Vertebrate sex steroid receptors: evolution, ligands, and neurodistribution. Ann N Y Acad Sci. doi: 10.1111/j.1749-6632.2009.04460.x.
- Thakur MK, Paramanik V. (2009) Role of steroid hormone coregulators in health and disease. Horm Res. doi: 10.1159/000201107.
- Casey G. (2017) Sex hormones and health. Nurs N Z.
Last Updated: May 31, 2022