Hemagglutination is a serological assay to identify a suspected virus and detect corresponding antibodies. The assay uses red blood cells as a source of antigens.
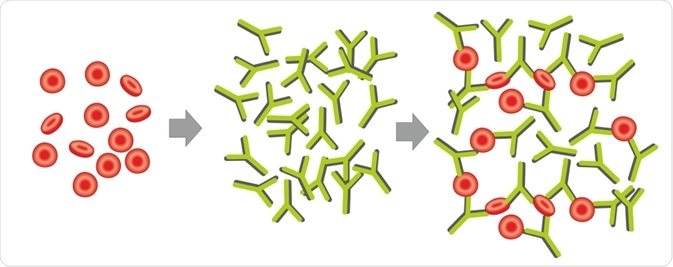 Image Credit: Soleil Nordic/Shutterstock.com
Image Credit: Soleil Nordic/Shutterstock.com
What is hemagglutination?
Hemagglutination is a reaction that causes clumping of red blood cells in presence of some enveloped viruses, such as the influenza virus. A glycoprotein on the viral surface, namely hemagglutinin, interacts with red blood cells, leading to the clumping of red blood cells and the formation of a lattice.
In absence of an enveloped virus, red blood cells precipitate at the bottom of a container, forming a red-colored dot. However, in presence of a virus, red blood cell clumps are dispersed, forming no red-colored dot. This is the basic principle of a hemagglutination assay.
How to perform a hemagglutination assay
To perform hemagglutination assay, biological samples containing viral particles are serially diluted (2-fold dilution) and dispensed into each well of a 96-well microtiter plate. Next, red blood cell aliquots are added to each well. The basic principle is that after a certain dilution, the red dot will appear at the bottom of the well.
The highest dilution of a given sample at which clumping is seen is considered as the hemagglutination titer. By multiplying the dilution fold, the viral titer can be determined. Generally, 1 hemagglutinin unit corresponds to 104 viral particles per milliliter of sample.
Hemagglutination is a widely used assay for detecting and titrating the influenza virus. One major benefit of this assay is that no specialized equipment is needed to perform the test. Although comes with relatively lower sensitivity, the assay can be used for robust and rapid detection of viruses.
What is a hemagglutination inhibition assay?
Hemagglutination inhibition assay (HIA) is used to detect and titrate antibodies developed against a virus. In HIA, an absence of hemagglutination is observed to detect the presence of antibodies in a given sample.
Mechanistically, virus-containing samples are incubated with serially-diluted serum samples. This allows the interaction between viral antigen and antibodies. Afterward, red blood cell aliquots are added to the reaction mixture. Viruses that have already formed a complex with antibodies will be unable to bind to red blood cells. This marks the absence of hemagglutination.
In the case of a known hemagglutinating virus, HIA can be used to detect antibodies. Conversely, in the case of an unknown virus, a panel of known antibodies can be used to identify the virus.
Although considered as a rapid and easy test to detect antibodies, HIA comes with certain disadvantages. For example, the assay cannot be used to detect antibodies that are not cross-reactive to the specific viral subtype tested. In this case, HIA should include all possible subtypes of a virus to effectively detect antibodies. This is not always possible to conduct.
Moreover, there are other aspects of adaptive immune responses against a virus, including T cell responses and antibody responses directed against viral components other than hemagglutinin protein. These components of the immune system cannot be detected using HIA.
What is a passive hemagglutination assay?
In passive hemagglutination assay, red blood cells generally collected from sheep, chicks, or humans are coated with antigen and incubated with biological samples to detect the presence of corresponding antibodies.
During incubation, antigens present in the sample competes with the antigen attached to the red blood cells for binding with corresponding antibodies that are also present in the sample. Afterward, the degree of hemagglutination is assessed to detect antibodies.
Conversely, red blood cells can be coated with a purified antibody to detect the microbial antigen in a given sample. This is called reverse passive hemagglutination. In this method, antibody-coated red blood cells are incubated with antigen-containing samples, and the degree of hemagglutination is assessed to detect the antigen.
Hemagglutination for blood typing
Before blood transfusion, ABO and Rh blood typing is performed to check the compatibility between the donor’s and recipient’s blood types. Besides pathogens, non-self blood types can also induce antibody production.
To test the donor’s and recipient’s blood types, recombinant antibodies developed against A, B, O, and Rh antigens are mixed with donor’s and recipient’s red blood cells, and hemagglutination is determined. In simple words, an A-positive blood sample will agglutinate with anti-A and anti-Rh antibodies.
A cross-match analysis is also carried out after the determination of blood type. In this case, the donor’s red blood cells are incubated with the recipient’s serum. In the recipient’s serum, the presence of antibodies against the donor’s red blood cells will result in hemagglutination.
 Image Credit: Cherries/Shutterstock.com
Image Credit: Cherries/Shutterstock.com
References
Last Updated: Mar 18, 2021