There are three bilaterally paired major salivary glands, the parotid, submandibular, and sublingual glands. In addition to these major glands, minor ones are located in the palate, lips, and buccal mucosa. Albeit a rare phenomenon, salivary gland neoplasms do occur.
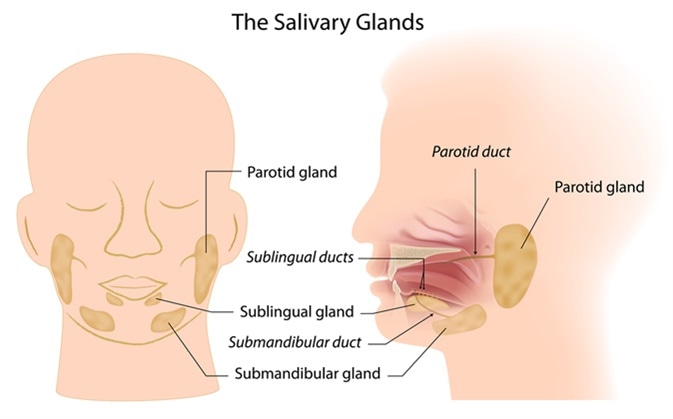
Salivary glands. Image Credit: Alila Medical Media / Shutterstock
In general, salivary gland neoplasms account for less than 5% of all head and neck cancers. They are more prevalent among women than men, and typically occur between the fourth and fifth decades of life. Benign salivary neoplasms represent a diverse group of tumors with a wide range of clinical behaviors.
Nearly three-fourths of salivary gland tumors arise in the parotid gland; most others arise from the minor salivary glands. Approximately 75% of parotid gland tumors are benign, but less than half of submandibular tumors are benign. Most neoplasms of the minor salivary glands are malignant. According to the World Health Organization, salivary gland tumors may be broadly classified as epithelial or non-epithelial. Because non-epithelial neoplasms are very rare (only 2% to 5% of salivary gland tumors), they will not be expounded upon herein. About one-third of epithelial-originating tumors are benign.
The World Health Organization lists several benign salivary gland tumors. The two most common of these are pleomorphic adenomas and Warthin tumors. The former accounts for up to 6 out of every 10 salivary gland neoplasms. Other benign epithelial salivary gland tumors are oncocytomas, cystadenomas, ductal papilloma, sebaceous adenomas, canalicular adenomas, lymphadenomas, myoepitheliomas, and basal cell adenomas.
Parotid Salivary Gland Tumor: Jubenal's Story
Clinical Presentation and Etiology
A patient with a salivary gland tumor may present with a swelling or lump in the vicinity of the jaw, neck, or mouth. This swelling may be accompanied by numbness and muscle weakness in the affected area. Additionally, the patient may have intractable pain, difficulty swallowing, and inability to fully open his or her mouth. Accompanying signs of xerostomia (dry mouth) may occur due to absent or reduced salivary flow from tumor blockage of the salivary duct.
The exact etiology of salivary gland tumors remains unknown. However, several genetic and environmental considerations that have been put forth. Smoking is believed to be closely associated with the development of Warthin tumors. Irritants in tobacco are thought to stimulate salivary gland metaplasia, which subsequently leads to neoplasia. Also implicated in these tumors is prior radiation exposure. Genetic aberrations have also been investigated for their potential role in the development of salivary gland neoplasms. Some other putative factors that may put persons at risk include viral infections, cell phone use, and occupational exposure to asbestos, nickel, or rubber.
Diagnosis and Treatment
In diagnosing neoplasms of the salivary glands, imaging studies are crucial. For major salivary glands, ultrasonography is an excellent modality to evaluate tumor morphology, size, and borders. Morphology can be characterized as solid, cystic, or complex, whereas borders are characterized as poorly defined or well-circumscribed. This type of imagining is crucial in establishing a diagnosis and choosing appropriate surgical therapy.
Further characterization of large tumors, which are more difficult to assess by ultrasound, or potentially malignant tumors may be done with the help of magnetic resonance imaging or computed tomography. Magnetic resonance imaging is particularly sensitive in establishing borders of soft-tissue tumors and invasion or spread to perineural areas. In some instances, fine-needle aspiration with biopsy is done to rule out other processes.
Surgical excision is usually employed to treat benign salivary tumors, barring any absolute contraindication. Following tumor removal, tumors may be further studied to establish a definitive diagnosis and determine if adjuvant treatment is needed. The most common benign salivary tumors, pleomorphic adenomas, have an excellent prognosis following removal, with only 3.4% and 6.8% recurrence at 5- and 10-year follow-ups, respectively. Other benign tumors of the salivary glands have similar prognoses, as they are generally cured following surgical excision.
References
Further Reading
Last Updated: Oct 24, 2018