Bladder cancer develops most commonly in the urothelial lining of the bladder. According GLOBOCAN database 2012, it is the 9th most common type of cancer worldwide, with 430,000 newly diagnosed cases in 2012.
What is Bladder Cancer?
Bladder cancer that originates from the urothelial lining is called urothelial or transitional cell carcinoma. This type of cancer is more common in males than females. The prevalence of bladder cancer is highest in Southern Europe, Western Europe and North America. However, the highest mortality rates are found in Western Asia and Northern Africa. Squamous cell carcinoma and adenocarcinoma are two other rarer forms of bladder cancer.
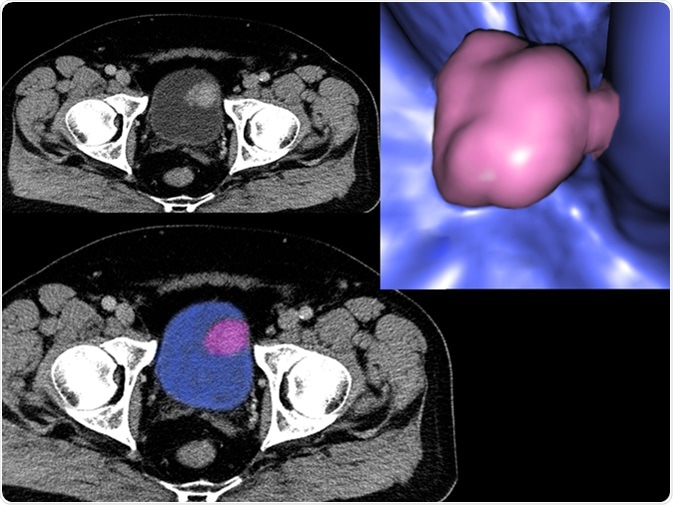
Image Credit: Semnic / Shutterstock
Stages and Grades of Bladder Cancer
Bladder cancers are categorized into different stages based on their invasiveness. Lesions that are restricted to the urothelium and do not invade any other muscle layer are grouped as non-muscle invasive bladder cancer (NMIBC). Carcinoma in situ or stage Tis, stage Ta (tumors of the mucosa), and stage T1 (tumors that invade the lamina propria) are included in NMIBC. In contrast to NMIBC, tumors that invade bladder wall muscle (stage T2), perivesical fat layer (stage T3), and nearby organs (stage T4) are grouped as MIBC.
Grading of bladder cancer in terms of cellular morphology is carried out based on the status of cellular differentiation; in which, grade 1 denotes well-differentiated tumors, grade 2 denotes moderately differentiated tumors and grade 3 denotes poorly differentiated tumors. Of these grades, poorly differentiated tumors are the most aggressive ones, which can potentially become invasive over time.
Bladder Cancer Genomics
Although the exact pathophysiology of bladder cancer is not known, mutations in genes that regulate important cellular events, such as cell division, growth, and survival, are significantly associated with the development of bladder cancer. These mutations are mostly somatic in nature, meaning that they are not inherited, rather, they are acquired during a person’s lifetime.
Bladder Cancer Genomic Research Study
Genes that are found to be significantly mutated in bladder cancer include:
Fibroblast growth factor receptor 3 (FGFR3) – this gene encodes a receptor tyrosine kinase called FGFR3, which plays an important role in regulating cell proliferation, cell type determination, blood vessel formation, and embryonic development. In some cases of bladder cancer, somatic mutation in FGFR3 gene causes overexpression of FGFR3 protein, which in turn results in tumor formation due to uncontrolled cell growth.
Epidermal growth factor receptor (EGFR) – this gene encodes a receptor tyrosine kinase called EGFR, which is found to be overexpressed in several bladder cancer cases due to genetic mutations. EGFR overexpression is also significantly associated with tumor progression and poor prognosis.
Epidermal growth factor receptor 2 (HER2) – this gene encodes a tyrosine kinase called HER2. Overexpression of HER2 is mostly found in high grade bladder cancers and is associated with an increased risk of tumor recurrence.
HRAS – this oncogene encodes a small GTPase protein called H-RAS, which is a member of the RAS superfamily. H-RAS acts by hydrolyzing GTP into GDP and primarily regulates cell growth. In some cases of bladder cancer, somatic mutation (gly12val) in HRAS gene leads to the formation of a constitutively active HRAS protein, which subsequently triggers rapid cell proliferation and induces tumor development. This mutation is also associated with bladder cancer progression, and thus, increases the risk of tumor relapse after treatment.
RB1 – this gene encodes a cell cycle regulator called pRB, which acts as a tumor suppressor by maintaining a tight control between cell division and DNA replication. This protein also regulates cell survival, apoptosis, and differentiation. Somatic mutation in RB1 gene, which makes this gene inactive, has been found in some cases of bladder cancer. Inactivation of RB1 gene downregulates the expression pRB protein and subsequently causes an abnormal cell growth and tumor formation.
TP53 – this gene encodes another cell cycle regulator called p53, which acts as a tumor suppressor. Upon DNA damage, p53 initiates cell cycle arrest and directs damaged cells to either DNA damage repair pathways or apoptotic pathways. Somatic mutation in TP53 gene is associated with bladder cancer development and progression.
Tuberous sclerosis complex 1 and 2 (TSC1/TSC2) – TSC1 gene encodes hamartin protein, and TSC2 encodes tuberin protein. TSC1/TSC2 complex acts as a tumor suppressor and negatively regulates mTOR signaling pathway. In some cases of bladder cancer, TSC1/TSC2 mutations result in increased PI3K/AKT/mTOR signaling and uncontrolled cell growth and survival as well as invasion.
Telomerase reverse transcriptase (TERT) – mutation in this gene has been found in 70% of bladder cancer cases. Protein encoded by this gene is known to be associated with DNA repair, aging process, and cancer development.
Further Reading
Last Updated: Oct 18, 2018