Histopathology provides a vast amount of valuable information about bladder cancer, such as the type, stage and grade of the cancer. This enables doctors to assess patient prognosis, best treatment options and possible specific therapies.
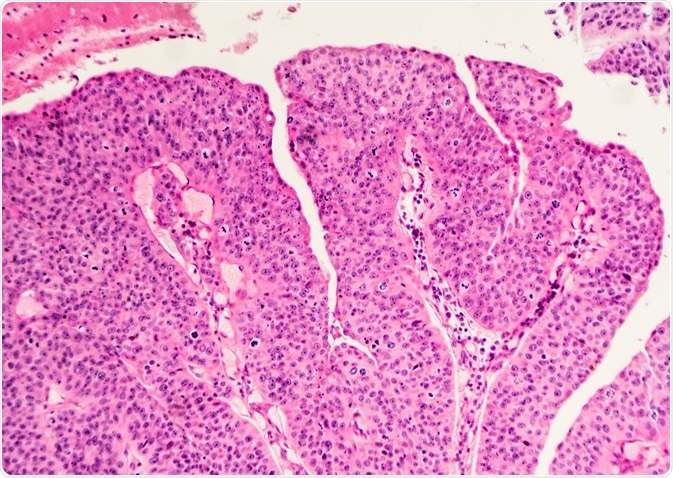 Image Credit: David Litman / Shutterstock
Image Credit: David Litman / Shutterstock
Histology of the bladder
The epithelium (cellular lining) of the bladder, as well as the pelvis, ureters and urethra, is called the urothelium. These cells have a very slow turnover rate of around 6 months and the number of layers in this lining varies depending on the fullness of the bladder. When full, it stretches to approximately 1 cell thick, whereas when empty, it bunches together to around 7 cells thick.
In bladder cancer, this slow and tightly controlled replication process is altered. The immortal cancer cells replicate constantly, evade cell death, induce angiogenesis, invade local tissue, and aggregate to form tumors.
There are also alterations within the nuclei and the cytoplasm of epithelial cells. These changes can be observed through histopathological evaluation and infer many specific properties of the cancer.
Histopathology and bladder tumors
The samples taken for histopathology have a great deal of variance, some are only small (3 mm) biopsies, whereas others are radical cystectomies. Evaluation of these samples can provide a vast amount of information about the specific tumor.
Type of cancer
Firstly, histopathology can provide information about the type of cancer. Previous research has led to extensive characterisation of many types of bladder cancer, including small cell, urothelial and squamous carcinomas.
There are a few types of urothelial bladder cancers. These occur in the lining of the bladder and account for over 90% of bladder cancers in the US and the UK. The first form of this cancer is non- muscle invasive bladder cancer. This type of bladder cancer is less aggressive than other types, and does not penetrate the wall of the bladder.
Non-muscle invasive bladder tumors are shaped like mushrooms, allowing for easy removal during surgery and thus, low reoccurrence rates. However, there are subtypes which can reoccur, including carcinoma in situ (CIS) and high grade T1 tumors. These cancers are flat, grow rapidly and metastasise into other tissues.
Squamous cell bladder cancers are highly invasive and originate from the squamous cells of the bladder. This form of bladder cancer is particularly prevalent in countries such as Egypt and African countries, due to the widespread infection of schistosomiasis.
Rarer types of bladder cancers include adenocarcinomas. These tumors originate from the mucosal cells lining of the bladder, which function to produce mucus. Commonly, they are very invasive, but they are also very rare. More rare examples of bladder cancers include sarcomas and small cell cancers.
These types of cancers all have different prognosis outcomes and specific treatment options, and therefore histopathology is very important for defining tumor type in bladder cancer.
Grading and typing of bladder cancers
Histopathology can also indicate the grade of cancer, which predicts how undifferentiated the tissue has become. WHO have a grading system in place which allows further categorization of cancers to improve the specificity of treatments.
This form of analysis can also indicate the pathological stage of the cancer, through tumor, node metastasis (TNM) staging. The T describes the size of the tumor and the level of infiltration into other cells, and is allocated a number on a scale of 1-4.
The N describes if the cancer has spread to the lymph nodes, and is allocated a number on a scale of 1-3. Finally, M indicates the level of total metastasis around the body and is either rated 0 (no metastasis) or 1 (metastasis).
For bladder cancer, there are various specific stages which are assessed through the analysis of TNM stages:
- Stage 0: Either a non-invasive papillary carcinoma or a carcinoma in situ
- Stage 1: Invaded the connective tissue
- Stage 2: Invaded the muscle
- Stage 3A: Invaded local tissues or one lymph node
- Stage 3B: Invaded >1 lymph node
- Stage 4A: Invaded pelvic or abdominal wall and lymph nodes away from the bladder
- Stage 4B: Metastasised
Overall, histopathology analysis provides lots of vital information about the cancer type, enabling doctors to improve prognosis through providing more specific and targeted treatment options.
Further Reading
Last Updated: Oct 10, 2022