Brain fog refers to impairments to thinking and concentration that may last a few hours or a few days that can negatively impact your life. Brain fog is commonly seen in anxiety, depression and menopause. COVID-19 may also cause brain fog in some cases, especially in those with more severe cases of the disease that can persist well after recovery of other symptoms.
 Image Credit: Hananeko_Studio/Shutterstock.com
Image Credit: Hananeko_Studio/Shutterstock.com
What is brain fog?
“Brain fog” is not strictly speaking a medical or scientific term; however, it refers to when individuals have issues with thinking and concentration, often leading to confusion, feeling disorganized, and poor memory recall with a lack of clear focus. Brain fog may only last a few minutes each time or can potentially last for several days at a time and may negatively impact your daily routine/activities of daily living.
There are many causes of brain fog including stress, anxiety, depression, lack of sleep, menopause and hormonal changes, hypothyroidism as well as certain medications and vitamin deficiencies (such as vitamin B12). In addition, certain diseases may also lead to brain fog which may include multiple sclerosis and fibromyalgia.
Brain fog in COVID-19
Whilst COVID-19 is primarily a respiratory disease, it can also have significant neurological effects such as the loss of the sense of taste/smell and headaches, for example. In the most severe cases, the lack of oxygen in the blood can have long-lasting negative consequences on the brain and other organs.
The exact prevalence of brain fog in COVID-19 is difficult to establish as it is not often the major symptom relating to COVID-19 and many people may not report it, especially outside of hospital settings. Furthermore, the majority of findings only come from hospitalized patients rather than non-hospitalized symptomatic patients (the majority of those that are affected).
However, according to one French study, as many as 28-34% of discharged COVID-19 patients had lingering issues with concentration issues and memory loss respectively. This was a small cohort of hospitalized patients, so these statistics may not reflect the global picture with respect to brain fog in COVID-19.
What causes brain fog in COVID-19?
This question has confused many scientists and clinicians and research into the exact mechanisms is still ongoing. One proposed mechanism is that SARS-CoV-2 leads to mitochondrial infection in the brain, leading to a proinflammatory response and hypoxia – which in itself favors viral replication. This leads to a toxic interaction between mitochondrial and viral genomes causing elevated brain infection, thus causing the array of psychiatric symptoms associated with COVID brain fog.
Energy-sensitive brain functions (i.e., cognition) can become functionally altered or disrupted due to energy imbalances caused by enhanced viral replication within the brain. As this leads to more hypoxia (the brain is more sensitive to hypoxia than most other organs), thus favoring more viral replication, this can lead to prolonged persistent brain fog effects even after the main respiratory symptoms have subdued.
An autopsy study from COVID-19 patients revealed none of the classic brain inflammation characteristics (including the presence of lymphocytes) associated with other viral diseases that affect the nervous system. Rather, they found megakaryocytes in brain capillaries – which is not commonly seen in the brain in similar diseases. These were present in around 1/3 of all deceased COVID-19 patients.
Megakaryocytes produce platelets (involved in blood clotting) and other blood cells in the bone marrow. Megakaryocytes, as the name suggests, are relatively large cells that are not typically found in capillaries, and their presence substantially affects flow within capillaries. Whilst the scientists behind this study do not assume megakaryocytes are the definitive cause of brain fog in COVID-19, their unusual presence may be linked to wider neurological and psychiatric symptoms and complications seen in COVID-19.
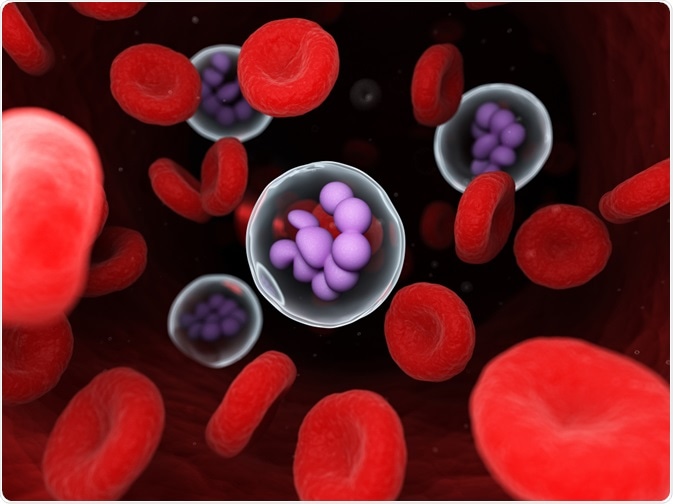 Image Credit: SciePro/Shutterstock.com
Image Credit: SciePro/Shutterstock.com
Brain fog is also seen in other neurological and degenerative diseases, so this may be a potential mechanism. However, other more traditional mechanisms may also be behind brain fog in COVID-19, such as inflammation, reduced tissue oxygenation, and reduced blood flow – potentially caused by infiltrating megakaryocytes. This needs further validation at present.
Brain fog may be directly related to COVID-19, but may also be related to the effects caused by COVID-19 such as poor sleep, etcetera. Thus, trying to get proper sleep is vital. Anti-inflammatories may also be useful in treating brain fog in COVID-19. Finally, brain fog can disappear on its own with the easing or passing of symptoms of COVID-19. If long COVID is present, it may take longer, and brain fog may be on the more prominent lingering symptoms of long COVID.
In summary, brain fog is a common umbrella term to describe a set of temporary cognitive symptoms including problems with thinking, memory and appearing confused. COVID-19 can sometimes lead to symptoms of brain fog, which may persist long after respiratory symptoms disappear. As this is currently a poorly understood mechanism in COVID-19, more research is needed to understand why this occurs and how we can treat it.
References
Further Reading
Last Updated: Mar 18, 2021