Breech presentation is common in about 15% of pregnancies at 29 to 32 weeks gestation. Although the breech position is common in the first two trimesters of pregnancy when the baby is more mobile, it is considered abnormal during late pregnancy. About 25% of breech babies undergo version and settle down in a head-first position by the time labor starts.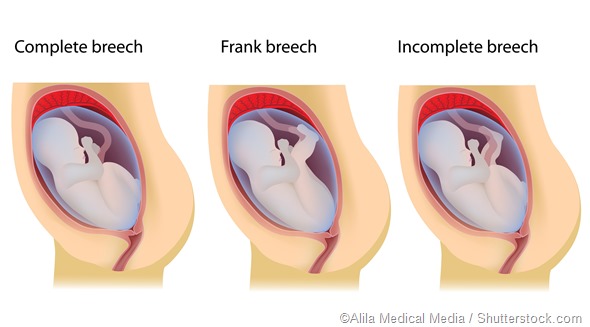
If a breech baby does not turn naturally, the treating healthcare providers might try turning the fetus through a process called external cephalic version. Here, the clinician applies pressure on the mother’s abdomen and tries to turn the baby into a head-first or cephalic position.
This procedure is successful in about 50% of breech babies. In situations where the external cephalic version is unsuccessful, the healthcare providers will need to prepare for breech birth. A cesarean section (c-section) is considered the safest method to deliver a breech baby, as there are some risks involved in the vaginal delivery of a breech baby.
Complications with vaginal breech delivery
Vaginal breech birth is complicated because during a head-down vaginal delivery the fetal head is delivered first. Being the largest part of a baby, the head expands the mother’s pelvis enough for the rest of the fetal body parts to be delivered.
However, in the case of a breech baby, the pelvis or hips are delivered first and the mother’s pelvis may not stay large enough for the fetal head that follows. The baby’s head can therefore get stuck in the birth canal, which results in serious complications that can cause serious injury or even death for the baby. Vaginal breech birth can also damage or block the umbilical cord, which will cut off the oxygen supply to the baby.
According to the Royal College of Obstetricians and Gynaecologists, vaginal breech delivery must be avoided in the following situations:
- Footling breech, which is when the feet of the baby are below its bottom
- The peculiar position of the fetus (i.e., the neck of the baby is tilted back)
- Large babies weighing over 3.8 kg
- Small baby weighing less than 2 kg
- Narrow pelvis with less space for the fetus to safely pass through the birth canal
- C-section delivery in a previous pregnancy
- Pre-eclampsia
- Low-lying placenta

Image Credit: Tinydevil / Shutterstock.com
Some serious complications related to vaginal breech delivery include:
- Trauma due to extended arm or head
- Placental detachment
- Injury to abdominal organs
- Broken fetal neck
- Umbilical cord prolapse leading to asphyxia
Vaginal breech delivery can still be safely performed by a skilled physician in the case of a complete breech or bottom-first position of the fetus if adequate pelvic room is available and the patient has not previously delivered a child by c-section.
C-section breech birth
A c-section is the only safe option in situations where there is a double footling breech, as well as when the mother has a small or narrow pelvis and a very large fetus. Planned c-section for breech birth has been found to lower both perinatal and neonatal death rates, lower short-term neonatal morbidity rates, and reduce 5 minute Apgar scores, as compared to vaginal breech births.
Decisions regarding the best mode of delivery for breech babies are made on an individual basis. In the case of women with breech presentation going into preterm labor, the recommended practice is to perform an emergency c-section. However, in case of fetal death inside the uterus or high maternal risk due to c-section, induction of labor and vaginal delivery is recommended. In modern clinical practice, a c-section is recommended for a transverse baby, regardless of whether the baby is alive or dead in the womb.
Some women go into labor after a c-section is planned. In such cases, depending on how close the baby is to being born, the healthcare provider makes a decision whether or not to proceed with the c-section. In some cases, if the baby is too close, a vaginal breech birth may be the safer alternative.
References
Last Updated: Mar 12, 2023