Smell loss (anosmia) is a common symptom of COVID-19 and occurs in a large proportion of infected patients even in the absence of any other symptoms such as fever or cough.
 Image Credit: Nenad Cavoski/Shutterstock.com
Image Credit: Nenad Cavoski/Shutterstock.com
Smell loss and COVID-19
Smell loss (anosmia), reduced smell (hyposmia) or altered smell are common features of colds and flu, in addition to sinusitis and allergies (e.g., hay fever). Smell loss is also associated with a large number of COVID-19 cases, even in the absence of fever and cough.
In addition, changes in taste are also commonly associated with smell loss in COVID-19. According to the NHS (UK), the 3 key symptoms of COVID-19 are: 1) fever, 2) new continuous cough & 3) smell and/or taste loss – and in some people, only 1/3 of these symptoms may be the only clinical presentation of COVID-19.
The exact prevalence of smell loss in COVID-19 varies considerably depending on different study estimates and cohort characteristics/demographics, however, estimates are thought to place smell loss in around 20-50% of all patients worldwide.
Other studies have shown that smell and taste loss in COVID-19 is more common in younger individuals compared to older patients and that there are no major differences between males and females, though some studies do suggest younger females with a higher BMI are at a higher risk.
Some studies have shown the prevalence of smell loss is higher in Western countries compared to East Asian countries – though this may be in part due to incomplete reporting of all symptoms, as well as some potential viral variant or host genetic differences.
A sudden loss of smell or taste has been linked to COVID-19, even in the absence of other symptoms such as fever and persistent cough. Smell loss for the majority of infected patients tends to be short-term (usually less than 2 weeks) and has a rapid recovery (within 10 days), though in some patients it can persist for much longer – especially with long-COVID.
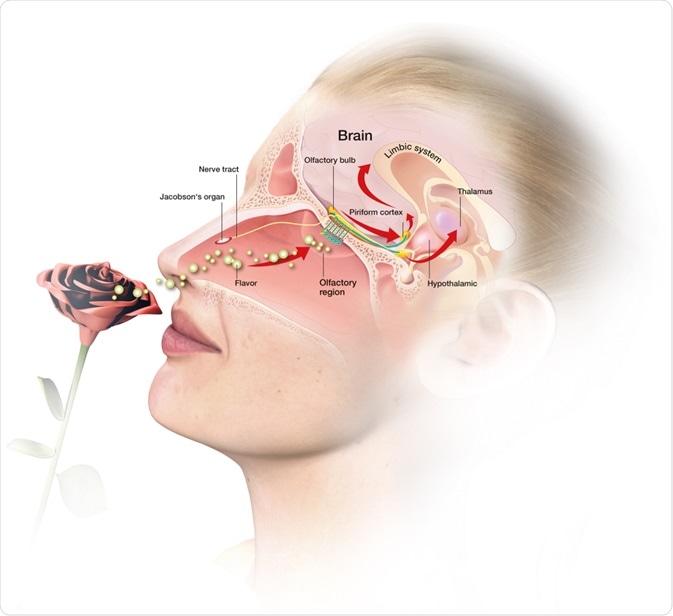
Unlike in colds and some flu cases where the cause of smell loss tends to be associated with stuffy noses (congestion caused by mucus build-up), in COVID-19 the sudden loss of smell may be directly related to SARS-CoV-2 infection within the nasal epithelium and olfactory neurons without any congestion.
Therefore, people with a sudden loss of smell should presume they are positive for COVID-19, take a PCR/lateral flow test to confirm and begin quarantining/self-isolating immediately.
How does smell loss in COVID-19 occur?
The mechanisms underlying smell loss in COVID-19 are still being fully explored as more research is done; however, some initial hypotheses and observations may explain why smell and taste loss occurs much more readily in COVID-19 even in the absence of other symptoms of nasal congestion compared to SARS, colds and flu.
In the small percentage of people who do develop nasal congestion and rhinorrhea, this physical obstruction of the nose with mucus would account for reduced smell (hyposmia). However, the majority of COVID-19 patients who suffer from smell loss typically do not get nasal congestion or rhinorrhea, and as such, other mechanisms must be involved.
So, what could be causing a sudden smell loss in COVID-19? Olfactory neurons do not seem to express SARS-CoV-2 binding receptors: ACE2 or TMPRSS2. Thus, a direct invasion of olfactory neurons in the nose or infiltration of the neurons in the olfactory bulb (brain) by SARS-CoV-2 is highly unlikely, and the presence of SARS-CoV-2 in the brain may be due to other routes such as trigeminal nerve endings.
However, despite olfactory neurons not expressing ACE2/TMPRSS2, another type of cell within the nose that sits next to olfactory neurons called sustentacular cells does express both ACE2 & TMPRSS2. These cells support olfactory neurons in the nose and can die as a result of infection.
Losing these cells does not however lead to the death of olfactory neurons but does cause sensory dysfunction (caused by cilia retraction) which may explain the sudden smell loss. Stem cells are able to quickly regenerate sustentacular cells which allow for the resumption of normal sensation within a week or two.
 3D illustration of the olfactory system. Image Credit: Axel_Kock/Shutterstock.com
3D illustration of the olfactory system. Image Credit: Axel_Kock/Shutterstock.com
When SARS-CoV-2 binds to ACE2/TMPRSS2 on sustentacular cells in the nose, these cells die leading to the loss of sensory cilia on olfactory receptor neurons. Consequently, odorants fail to bind to neurons’ cilia thus causing anosmia to occur. All of this can happen very rapidly in as little as 1 or 2 days.
Whilst this occurs, stem cells are able to quickly regenerate sustentacular cells (usually within 3-7 days), allowing for cilia on olfactory neurons to regenerate allowing odorants to once again bind to neurons and the sense of smell recovers (within another day or two). This explanation is consistent with the typical time course of sudden anosmia in COVID-19, as well as its rapid recovery.
In the small proportion of COVID-19 patients who suffer anosmia for several weeks or possibly months, there could be additional factors in play. It may be that a larger area of the nose is affected with more sustentacular cells damaged with the possibility of the death of olfactory neurons (which take much longer to regenerate). Some patients may also suffer from cytokine storms (including high levels of TNF-alpha) which can also lead to the death of neurons.
Summary
In summary, sudden smell loss (anosmia) is a common symptom of COVID-19 which may occur without any other symptoms (such as fever or cough). Unlike other respiratory conditions where the reduced smell is usually a result of nasal congestion, in COVID-19, the vast majority of affected patients do not have nasal congestion.
Olfactory neuronal dysfunction caused by the death of sustentacular support cells (due to SARS-CoV-2 invasion) may be the cause of anosmia in COVID-19, and their subsequent regeneration within a week or so may allow for the rapid recovery seen in many patients worldwide.
References
Further Reading
Last Updated: Apr 19, 2021