What is candida, and why is it in your gut?
What causes candida overgrowth in the gut?
Common symptoms of candida overgrowth in the gut
Risk factors for developing candida overgrowth
Diagnosing candida overgrowth: How is it identified?
The impact of candida overgrowth on gut health
Managing candida overgrowth: Treatment and prevention
Conclusion
References
Further reading
What is candida, and why is it in your gut?
The human vagina and digestive tract naturally contain Candida albicans, with the digestive system considered the main infection reservoir. 1-4 The gut microbiota is recognized as the primary internal source of both disseminated candidosis and candidaemia. 4
An estimated 1.5 million deaths worldwide are attributed to invasive fungal diseases annually. 5 Of these, hospital-acquired infections—most frequently caused by species of Candida—account for around 80% of the deaths resulting from fungal sepsis. 6
In individuals with compromised immune systems, Candida albicans is more likely to enter the bloodstream and cause widespread candidiasis, which is why invasive candidiasis more frequently affects AIDS and intensive care unit patients. 7-9
The dimorphic fungus Candida albicans normally coexists on the skin as a benign commensal but has the potential to become pathogenic. It frequently causes diseases, including diaper rash, paronychia, and onychomycosis, by infecting skin folds like the groin, underarm, and armpits. Yeast forms enter the epidermis during infection, while filamentous forms penetrate deeper into the dermis.10
 Candida fungi. Image Credit: Kateryna Kon/Shutterstock.com
Candida fungi. Image Credit: Kateryna Kon/Shutterstock.com
At least fifteen different species of candida are known to cause disease in humans, although the five most prevalent pathogens—Candida albicans, Candida glabrata, Candida tropicalis, Candida parapsilosis, and Candida krusei—account for more than 90% of invasive diseases. Although each of these species has a distinct epidemiology, pathogenicity potential, and susceptibility to antifungals when combined, serious infections caused by these organisms are typically referred to as invasive candidiasis. 12
What causes candida overgrowth in the gut?
A nonkeratinized stratified squamous epithelium that is a component of the innate immune barrier normally guards the esophagus. About 20% of people may have a colonization of Candida albicans in their esophagus; however, immune system dysfunction or localized esophageal lesions may cause the yeast to overgrow and produce yellow-white patches. These plaques, which are seen during upper endoscopy, cannot be removed and may either stay in one place or spread throughout the esophagus. 13,14
Normally, immunological responses within the digestive tract stop overgrowth of fungi. On the other hand, alterations in gut flora and gene regulation raise the risk of opportunistic fungal infections in cases of immune system weakness or following antibiotic usage. Due to its ability to stick to tissues and create enzymes that dissolve barriers, candida thrives. Low immunity, improper use of antibiotics, chemotherapy, and endocrine or nutritional problems are some of the contributing causes to candida's growth. 15,16
Common symptoms of candida overgrowth in the gut
Some common signs and symptoms often observed in patients include diarrhea, abdominal pain, nausea, bloating, and cramps, among others. 17,18 Candida colonization has been shown to occur in GI tract disease patients in a number of circumstances, including Crohn's disease, ulcerative colitis, gastric ulcers, duodenal ulcers, and perforated ulcers.19
Risk factors for developing candida overgrowth
The three main risk factors for GI candidiasis are radiation, intestinal inflammation, and recurrent GI surgery. A diet heavy in protein had the opposite impact from one high in carbohydrates, which raised the overall number of candida species. 20
Candida albicans spontaneously colonize the mucosa of the esophagus, oropharynx, and gastrointestinal system in healthy persons. However, it can cause mucosal candidiasis in these areas, particularly in immunocompromised individuals. Immune system suppression due to conditions like leukemia and lymphoma, or the use of cytotoxic drugs and corticosteroids, increases vulnerability to candida infections. 21
Antibiotic use can also lead to candidiasis by disrupting the natural balance of bacterial flora, allowing candida to overgrow. Additionally, fungal translocation through impaired mucosal barriers may result in candida-related fungemia, especially in cancer patients undergoing cytotoxic chemotherapy.
Though candida is typically a commensal organism, changes in the host environment and bacterial populations in the gastrointestinal tract can turn it into an opportunistic pathogen. 21
Diagnosing candida overgrowth: How is it identified?
The diagnosis of a candida infection, which often requires histological evidence, cannot be made solely by isolating candida from sputum and stool specimens, as candida is a normal component of the mycotic flora in the oral and gastrointestinal tracts.
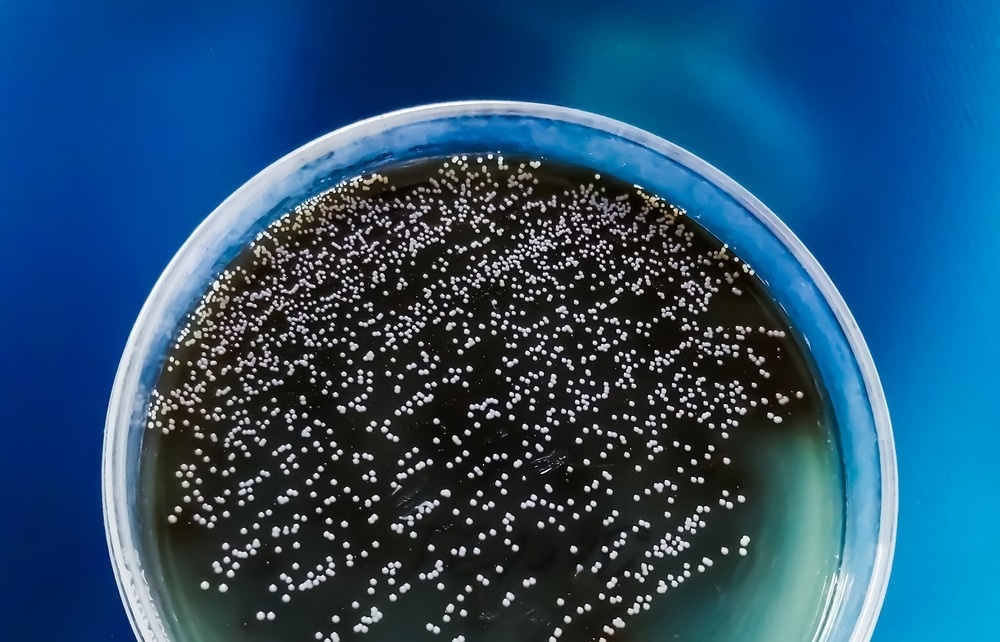 Colonies of Candida albican from urine sample on agar media plate. Image Credit: Saiful52/Shutterstock.com
Colonies of Candida albican from urine sample on agar media plate. Image Credit: Saiful52/Shutterstock.com
Tissue from an endoscopic biopsy may exhibit pathological characteristics, including multiple abscesses and an acute inflammatory response. Pseudohyphae and fungal spores are typically observed, with neutrophils predominating. 17
Diagnosis should be considered if patients exhibit typical clinical signs. Candida is found in microbiological cultures, and significant risk factors exist, such as the use of corticosteroids, immunosuppressive medications, or broad-spectrum antibiotics. 17
Clinical symptoms and notable growth of Candida albicans in cultures are required for the diagnosis of mucosal candida infections. For instance, the alleviation of dysphagia and substernal pain that occurs after systemic anticandidal therapy is indicative of candidal esophagitis. Because dysphagic individuals run the danger of developing strictures, esophagoscopy is advised.
When stomach discomfort and meteorism respond to treatment similarly, it could be a sign of intestinal candidiasis. Strong signs of infection also include an abundance of growth on fecal cultures and a stool smear with Candida mycelia. Interestingly, intestinal and esophageal candidiasis can develop without mouth irritation. 22
The impact of candida overgrowth on gut health
Candida organisms are normally benign and are a regular component of the human gut microbiota. However, recent studies have linked elevated levels of candida colonization with gastrointestinal disorders.
Research in animal models suggests that candida impedes the healing of inflammatory lesions while inflammation promotes further colonization. Patients with inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis, show significantly higher levels of candida colonization.
Furthermore, candida organisms are frequently cultured from stomach biopsies, mucosal brush samples, or peritoneal fluid in various studies, and they are commonly found in ulcers, particularly large or perforated ones. 19
Managing candida overgrowth: Treatment and prevention
Nystatin is used as a three- to six-week treatment for intestinal candidiasis. The dosage is 100,000 IU/L of drinking water and 200,000 IU/kg of soft food. Amphotericin B can be applied topically and intravenously to treat dermatitis and ocular diseases. It's important to treat the predisposing variables as well. 23
Probiotics may help shield kids from developing invasive candidiasis and candida colonization, according to a number of studies. One study showed that a combination of probiotics (Bifidobacterium longum, Bifidum, B. acidophilus, and Bifidum lactis) was given to preterm infants and neonates, and these individuals had considerably shorter hospital stays and less enteral yeast colonization than a control group.
Another assessed the effectiveness of probiotics in a pediatric intensive care unit and found that children receiving probiotics while on broad-spectrum antibiotics showed a relative drop in candida colonization, with decreases of 34.5% on day 7 and 37.2% on day 14. These results imply that giving critically ill children probiotic supplements may successfully reduce the amount of gastrointestinal candida infection. 20
Foods heavy in sugar and fat with little vegetable fiber have a detrimental effect on gut microbiota. This leads to dysbiosis and an overabundance of Candida albicans, a major cause of fungal infections worldwide.
In addition, long-term antibiotic usage, chronic psychological stress, sedentary lifestyles, smoking, and excessive alcohol intake all contribute to the development of illness and dysbiosis in the gut. 24
On the other hand, a varied diet high in micronutrients from probiotic or prebiotic supplements, vegetable fiber, omega-3 polyunsaturated fatty acids, vitamins D and E, and other nutrients can decrease fungal species in the gut, increase the diversification of the microbiota, and encourage the synthesis of short-chain fatty acids. 24
Garlic has been demonstrated to have antifungal effects against Candida albicans, while powdered and liquid lemongrass also possesses antifungal characteristics. Moreover, oleic acid exhibits antifungal properties against Candida krusei and Candida albicans, and ginger extract can prevent the production of biofilms by these two types of candida. 24
Conclusion
In conclusion, while Candida albicans is a normal inhabitant of the human gut and plays a role in maintaining gut health, an overgrowth can lead to significant health issues, particularly in immunocompromised individuals.
Factors such as antibiotic use, dietary influences, and underlying health conditions contribute to the risk of candida overgrowth, potentially resulting in invasive candidiasis and various gastrointestinal disorders.
Effective management strategies, including antifungal treatments and the use of probiotics, show promise in preventing and reducing candida colonization and its associated complications.
Continued research is essential to fully understanding the dynamics of candida in the gut and developing effective prevention and treatment strategies.
References
- Odds, F. C. (1988). Candida and candidosis: a review and bibliography (pp. x+-468pp). https://www.cabidigitallibrary.org/doi/full/10.5555/19892057780
- Gow, N. A., van de Veerdonk, F. L., Brown, A. J., & Netea, M. G. (2011). Candida albicans morphogenesis and host defence: discriminating invasion from colonization. Nature Reviews. Microbiology, 10(2), 112–122. https://doi.org/10.1038/nrmicro2711
- Poulain, D., Sendid, B., Standaert-Vitse, A., Fradin, C., Jouault, T., Jawhara, S., & Colombel, J. F. (2009). Yeasts: neglected pathogens. Digestive Diseases (Basel, Switzerland), 27 Suppl 1, 104–110. https://doi.org/10.1159/000268129
- Poulain D. (2015). Candida albicans, plasticity and pathogenesis. Critical Reviews in Microbiology, 41(2), 208–217. https://doi.org/10.3109/1040841X.2013.813904
- Brown, G. D., Denning, D. W., Gow, N. A., Levitz, S. M., Netea, M. G., & White, T. C. (2012). Hidden killers: human fungal infections. Science Translational Medicine, 4(165), 165rv13-165rv13. https://pubmed.ncbi.nlm.nih.gov/23253612/
- Biswas, P. S. (2021). Vaccine-induced immunological memory in invasive fungal infections–a dream so close yet so far. Frontiers in Immunology, 12, 671068. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.671068/full
- Kett, D. H., Azoulay, E., Echeverria, P. M., & Vincent, J. L. (2011). Candida bloodstream infections in intensive care units: analysis of the extended prevalence of infection in intensive care unit study. Critical Care Medicine, 39(4), 665-670. https://pubmed.ncbi.nlm.nih.gov/21169817/
- Mohd Badri, P. E. A., Rismayuddin, N. A. R., Kenali, N. M., Darnis, D. S., & Arzmi, M. H. (2022). Characterization of Cervus timorensis velvet antler and its effect on biofilm formation of Candida species. Medical Mycology, 60(9), myac073. https://pubmed.ncbi.nlm.nih.gov/36099875/
- Mikulska, M., Magnasco, L., Signori, A., Sepulcri, C., Dettori, S., Tutino, S., ... & Bassetti, M. (2022). Sensitivity of serum beta-D-glucan in candidemia according to Candida species epidemiology in critically ill patients admitted to the intensive care unit. Journal of Fungi, 8(9), 921. https://pubmed.ncbi.nlm.nih.gov/36135645/
- Gow, N. A., Van De Veerdonk, F. L., Brown, A. J., & Netea, M. G. (2012). Candida albicans morphogenesis and host defence: discriminating invasion from colonization. Nature Reviews Microbiology, 10(2), 112-122. https://www.nature.com/articles/nrmicro2711
- Havlickova, B., Czaika, V. A., & Friedrich, M. (2008). Epidemiological trends in skin mycoses worldwide. Mycoses, 51, 2-15. https://pubmed.ncbi.nlm.nih.gov/18783559/
- Pappas, P. G., Kauffman, C. A., Andes, D., Benjamin, D. K., Jr, Calandra, T. F., Edwards, J. E., Jr, Filler, S. G., Fisher, J. F., Kullberg, B. J., Ostrosky-Zeichner, L., Reboli, A. C., Rex, J. H., Walsh, T. J., Sobel, J. D., & Infectious Diseases Society of America (2009). Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 48(5), 503–535. https://doi.org/10.1086/596757
- Vermeersch, B., Rysselaere, M., Dekeyser, K., Rasquin, K., De Vos, M., Elewaut, A., & Barbier, F. (1989). Fungal colonization of the esophagus. The American Journal of Gastroenterology, 84(9), 1079–1083. https://pubmed.ncbi.nlm.nih.gov/2570525/
- Klotz, S. A. (2006). Oropharyngeal candidiasis: a new treatment option. Clinical Infectious Diseases, 42(8), 1187-1188. https://academic.oup.com/cid/article/42/8/1187/283188
- Levine, M. S., Macones, A. J., Jr, & Laufer, I. (1985). Candida esophagitis: accuracy of radiographic diagnosis. Radiology, 154(3), 581–587. https://doi.org/10.1148/radiology.154.3.3969456
- Vazquez J. A., Sobel J. D. Candidiasis. In: Dismukes W. E., Pappas P. G., Sobel J. D., editors. Clinical Mycology. New York, NY, USA: Oxford University Press; 2003. pp. 143–187.
- Mohamed, A. A., Lu, X. L., & Mounmin, F. A. (2019). Diagnosis and Treatment of Esophageal Candidiasis: Current Updates. Canadian Journal of Gastroenterology & Hepatology, 2019, 3585136. https://doi.org/10.1155/2019/3585136
- Knapp, K. M., & Flynn, P. M. (2009). Candidiasis. In R. D. Feigin, J. D. Cherry, G. J. Demmler-Harrison, & S. L. Kaplan (Eds.), Feigin and Cherry's Textbook of Pediatric Infectious Diseases (6th ed., pp. 2741-2751). W.B. Saunders. https://doi.org/10.1016/B978-1-4160-4044-6.50217-X
- Kumamoto C. A. (2011). Inflammation and gastrointestinal Candida colonization. Current Opinion in Microbiology, 14(4), 386–391. https://doi.org/10.1016/j.mib.2011.07.015
- Andrade, J. C., Kumar, S., Kumar, A., Černáková, L., & Rodrigues, C. F. (2022). Application of probiotics in candidiasis management. Critical Reviews in Food Science and Nutrition, 62(30), 8249–8264. https://doi.org/10.1080/10408398.2021.1926905
- R AN, Rafiq NB. Candidiasis. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560624/
- Perheentupa, J. (2002). APS-I/APECED: The clinical disease and therapy. Endocrinology and Metabolism Clinics of North America, 31(2), 295-320. https://doi.org/10.1016/S0889-8529(01)00013-5
- Dorrestein, G. M. (2009). Passerines. In T. N. Tully, G. M. Dorrestein, A. K. Jones, & J. E. Cooper (Eds.), Handbook of avian medicine (2nd ed., pp. 169-208). W.B. Saunders. https://doi.org/10.1016/B978-0-7020-2874-8.00008-0
- Jawhara S. (2023). Healthy Diet and Lifestyle Improve the Gut Microbiota and Help Combat Fungal Infection. Microorganisms, 11(6), 1556. https://doi.org/10.3390/microorganisms11061556
Last Updated: Oct 16, 2024