Intrauterine insemination (IUI) is a technique of assisted conception, in which washed and sorted motile sperm are inserted through the uterine cervix into the uterine cavity to increase the chances of natural fertilization of the oocyte within the fallopian tubes. An IUI is indicated in severe or moderate male factor infertility and in mild unexplained infertility.
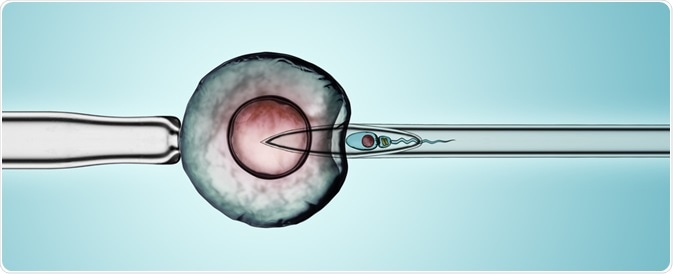
Image Credit: Nixx Photography / Shutterstock.com
The chances of success for an IUI are dependent upon several factors. The live birth rate is lower than the pregnancy rate and, therefore, the success rates published by various centers should be evaluated accordingly.
Prognostic factors
Cause of infertility
First of all, conception rates depend, though marginally, on the reasons for infertility. The duration of infertility also plays a role. Infertility due to anovulation or unexplained infertility is somewhat more easily treated with IUI as compared to infertility cases that are due to endometriosis or male factor infertility.
Ovarian hyperstimulation
Whether or not medications are used to induce ovulation and the type of protocol used may have an effect on the success rates. The follicular response and increase in endometrial thickness following the induction of ovulation may also act as prognostic markers.
Many centers have reduced the dosage of drugs used to stimulate the ovaries because of the high risk of multiple pregnancies with these protocols. Superovulation is often associated with double or triple the pregnancy rates, as well as an increase in the number of multiple pregnancies. This can be as high as 20% for twins, and 40% for higher-order gestations. Ovarian hyperstimulation syndrome is also a foreseeable risk with increasing numbers of preovulatory follicles.
Age
The age of the woman undergoing the IUI procedure significantly affects how well it will work. Women who are below the age of 40 years, in general, have a more than 50% chance of achieving pregnancy after six cycles of IUI, with a success rate of over 75% after 12 cycles. Some other sources put the cumulative pregnancy rate at 20-33% following six cycles of ovarian hyperstimulation with IUI.
The importance of the woman's age lies in the well-established reduction in oocyte quality as age increases, which is not offset by overcoming barriers to fertilization. IUI success rates start to decline even after the age of 35 years.
For women above 40 years, live births may occur in only about 1.5% of women who have undergone IUI treatment cycles. For these reasons, this is a poor option for women older than 40 years, and even after the age of 35, this procedure should be offered with extreme caution.
Semen parameters
Sperm count and sperm preparation techniques may make a difference in the ease of conception with IUI.
The use of fresh sperm, for example, has a higher conception rate as compared to the use of frozen and thawed sperm. Certain sperm characteristics will also affect pregnancy rates, including the total motile fraction (TMF), the morphology, and the motility of the washed sperms.
The TMF significantly increases the pregnancy rate to almost double, when it is between 10 and 20 million. However, its reduction to less than 10 million is associated with low success rates. Additionally, TMF counts over 20 million are also associated with a reduction in pregnancy success rates, though the reason for this latter finding is unknown.
Even within this classification, a TMF of less than 1 million has been linked to disappointing rates. Comparatively, the success of a TMF of less than 5 million can be successful; however, this is largely dependent upon the sperm morphology. The success rate of a TMF of less than 5 million is about 6% when abnormal sperms are abundant, which is comparable to a success rate of almost 20% when normal morphology is present in most sperms.
IUI - Fertility expert secrets for maximum pregnancy rates
Timing and number of inseminations
If the timing of ovulation is not correctly detected, the time of insemination may not be synchronized with the period of peak female fertility within the cycle. Thus, the appropriate techniques for determining whether ovulation has occurred or not must be utilized.
A premature LH surge occurs in many cases, from a quarter to a third of treated women, which reduces the pregnancy rates. The use of LH antagonists or clomiphene citrate to prevent an early surge is currently being studied for its ability to increase the success rates of IUIs.
The number of inseminations within a cycle is also an important factor in determining the success rate of an IUI. If insemination is repeated twice within the same cycle, the number of pregnancies may increase.
Donor sperm
Successful insemination with donor sperm is also dependent upon the age of the woman. Overall, donor sperm used for IUIs is associated with a 22% conception rate per cycle, which is comparable to less than 10% when only homologous sperm are used.
The use of donor sperm has resulted in the following per cycle live birth rates:
- Under 35 years - about 16%
- 35 to 39 years - 11%
- 40 to 42 years - >5%
- 43 to 44 years - <1%
- Over 44 years - 0%
However, higher rates have been reported in the United States, with 10-15% live births reported in the 41-42 year age group, and successfully pregnancies in about 5% of women older the age of 42.
Importance
It is important to establish robust prognostic factors, as these can help formulate guidelines to make IUI more focused on its application. This will increase live birth rates and reduce the number of unhelpful IUIs performed.
For instance, couples with male factors predominating as a cause of infertility, females over the age of 40, and sperm samples with a TMF below 5 million, would be ideal for in vitro fertilization rather than an IUI. Considering the low pregnancy rates per cycle, many couples might prefer to attempt another more effective procedure once than undergo the emotional, physical, and financial strain of repeated IUI cycles, especially when they live in remote locations.
References
Further Reading
Last Updated: Sep 2, 2022