White cells are the immune cells of the body. Also called leukocytes, they are useful in fighting infections and belong to five types. About 100 million white cells are produced by the body each day.
These include granulocytes, comprising neutrophils, basophils, and eosinophils, and the non-granular cells, comprising lymphocytes and monocytes. The former are produced in the bone marrow, as are monocytes, while the lymphocytes are produced in the lymphoid tissue.
Neutrophils makeup 45-75% of white cells in the circulation, and are the major first-line defense against infectious pathogens such as bacteria and some fungi. Lymphocytes make up 20-40%, with other white cells comprising small percentages.
A normal white cell count is between 4,000 to 11,000 cells per microliter of blood. Counts that are higher or lower than expected could indicate an underlying health condition. A higher count is referred to as leukocytosis, while low counts are called leukopenia.
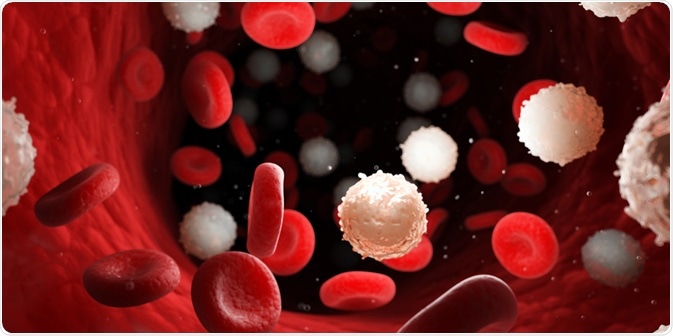
Image Credit: SciePro/Shutterstock.com
Causes of leukocytosis
Leukocytosis is defined as a white blood cell count greater than 11,000 per microliter of blood.
Leukocytes are raised in most infections and inflammatory conditions. Other causes may exist, such as the use of corticosteroids, lithium, and beta-agonists. The highest rise is seen with serious disorders such as leukemias, which are cancers of the bone marrow. In these conditions, immature white cells are sometimes released too early from the bone marrow, causing a shift to the left.
With marked leukocytosis in the absence of a discoverable infection, injury, or inflammation, a sample of blood is viewed under the microscope to look for immature cells, or myeloblasts. This is especially so if red cells and platelet are also abnormal.
The most common bone marrow disorders include acute leukemias, chronic leukemias, and myeloproliferative disorders.
An increase in the white cell count may involve one or more types of cell. When only the neutrophils are involved, it is called neutrophilic leukocytosis, while with a predominance of lymphocytes, lymphocytic leukocytosis is present.
Eosinophilia is defined as a peripheral blood eosinophil count > 500/microliter. Eosinopenia is not usually considered a problem though it may occur during Cushing’s syndrome, sepsis, and corticosteroid treatment.
Monocytes make up 1-10% of the blood cells, while basophils comprise <3%. Eosinophils make up less than 7%.
Causes of leukopenia
Leukopenia is a decrease in the number of white blood cells to fewer than 4,000 cells per microliter of blood.
Neutropenia is defined as a drop in circulating neutrophils below 1,500/microliter in Whites, but <1,200/microliter in Blacks.
Lymphocytopenia is referred to as <1,000 lymphocytes/microliter in adults, but since these cells comprise only 20-40% of the total white cell count, a drop in the total count is not always present.
Monocytopenia refers to the presence of <500 monocytes/microliter. These cells migrate into the tissues, where they become macrophages, engulfing and destroying foreign bodies and pathogens, as well as cell debris.
Low white cell counts may be caused by the underproduction of white cells in the bone marrow, sometimes following exposure to chemicals like benzene, or due to primary or secondary malignancies. The treatment of cancers by chemotherapy or radiation can also cause leukopenia due to reduced bone marrow synthesis of these cells.
Autoimmune disorders such as systemic lupus erythematosus, or rheumatoid arthritis, can also lead to the destruction of the body’s own white cells by antibodies created by the immune system.
Viral infections may also cause leukopenia, usually because of the rapid consumption of white cells faster than the rate of their production in the bone marrow. The human immunodeficiency virus (HIV) is known to target one type of lymphocyte, bearing the CD4 marker, leading to profound immunodeficiency.
Drugs such as some antibiotics are known to cause leukopenia by the destruction of white cells.
The presence of generalized malnutrition, or the deficiency of certain vitamins such as folic acid and vitamin B12 can also affect bone marrow production of white cells. This is the case with alcohol intake in excess as well because this can be associated with the deficiency of some B vitamins.
Hypersplenism is another cause of leukopenia since it is a source of lymphocytes. When hit by infections, clots, or disease, it can stop producing enough white cells.
These conditions are diagnosed in part by a differential count of the five types of white cells, indicating a higher possibility of a viral or bacterial infection, an allergy, or the presence of inflammation.
Neutrophil abnormalities
Neutrophilic leukocytosis is seen in infections when the body fights off invading pathogens or reacts to foreign particles. Bacteria, viruses, fungi, and parasites may all trigger such a rise.
It is also observable after injuries, during inflammatory disorders, and with the use of certain drugs like corticosteroids. The most alarming rise is typically seen with myeloid leukemias, with acute myeloid leukemia being associated with a higher percentage of immature cells in the blood.
Neutropenia is a potentially life-threatening condition. The most common cause is cancer chemotherapy or radiation.
The occurrence of frequent or unusual infection often raises the suspicion of neutropenia, which is diagnosed with a blood test, and sometimes a bone marrow biopsy.
Neutrophils may be decreased due to underproduction or over-consumption. The former may occur due to cancers of the bone marrow, influenza and other viral infections, tuberculosis and other bacterial infections, myelofibrosis where the bone marrow is replaced by fibrous tissue, or deficiencies of vitamin B12 or folate, as mentioned above.
Drugs, radiation, and chemotherapy are also causes of acute neutropenia. Some uncommon hereditary disorders such as cyclic neutropenia and chronic benign neutropenia are also known, as well as severe congenital neutropenia, a cluster of illnesses where neutrophils fail to mature, leading to high susceptibility to severe infections.
Lymphocytic leukocytosis
In this condition, total white cell counts are up because of increased numbers of lymphocytes. These cells protect against all types of pathogens. They are of three types, B cells, T cells, and Natural Killer (NK) cells.
Lymphocytosis occurs most commonly in viral infections like infectious mononucleosis, lymphomas, and lymphocytic leukemias. Certain autoimmune diseases may also be associated with increased lymphocyte counts.
Monocyte abnormalities
Low monocyte counts can be associated with a high risk of infection, which can be serious in patients with acetaminophen-induced liver damage, or burns. The causes include myelosuppression due to chemotherapy, certain mutations of the bone-forming cells, cancers of the lymphoid system, infections, treatment with steroids or immunoglobulins, and certain surgeries.
Monocytosis can occur with infectious mononucleosis, mumps, and measles, certain parasitosis, chronic infections, acute stress or trauma, systemic inflammations including autoimmune disorders, drug reactions, neutropenia, and after splenectomy.
Eosinophil abnormalities
Eosinophils are involved in primary defenses against parasitic infections, though their exact role is not clear. Raised eosinophil counts, therefore, indicate the presence of parasites, intracellular bacteria, or an allergic reaction, among many other conditions.
Prolonged eosinophilia is associated with tissue damage. The presence of Charcot-Leyden crystals, composed of phospholipase B
Eosinophil counts may go down with stress, with the use of beta-blockers, or corticosteroids. Some bacterial or viral infections also cause eosinopenia.
Basophil abnormalities
Basophil counts go down in thyrotoxicosis, acute allergies, and infections. Basophilia may be observed in hypothyroidism, myeloproliferative disorders, such as polycythemia vera. Increased basophil counts can cause itching in some cases.
References:
Further Reading
Last Updated: Dec 7, 2021