Mucormycosis is a rare but highly deadly fungal infection that most commonly affects immunocompromised individuals, particularly those with diabetes mellitus.
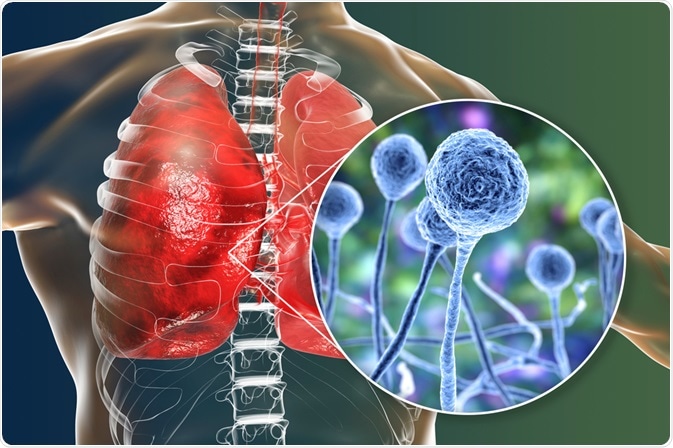
Mucormycosis. Image Credit: Kateryna Kon/Shutterstock.com
What is mucormycosis?
Mucormycosis is a life-threatening fungal infection that typically affects immunosuppressed individuals, such as those with hematological malignancies like leukemia and lymphoma, stem cell transplant recipients, and diabetes mellitus (DM). Although DM is the most predominant underlying medical comorbidity in patients who are diagnosed with mucormycosis, the incidence of this fungal infection has increased in patients with varying causes of both innate and acquired immunosuppression. This rise in mucormycosis cases is likely to be multifactorial.
The Mucorales fungi are responsible for mucormycosis, with the Rhizopus, Mucor, and Rhizomucor organisms often being responsible for human infections. To cause infection, these fungal spores will typically enter the respiratory tract through inhalation; however, they can also enter host cells through the skin as a result of trauma or through accidental ingestion.
Rhino-orbital-cerebral mucormycosis
As previously mentioned, patients with DM are at the highest risk of developing mucormycosis. More specifically, the most frequent presentation of this fungal infection in patients with DM is rhino-orbital-cerebral mucormycosis. This specific type of fungal infection is one of three types of rhinocerebral mucormycosis, in addition to rhinomaxillary and rhino-orbital mucormycosis.
Some of the symptoms that are commonly associated with these types of rhinocerebral mucormycosis include rhinorrhea, headaches, necrotic areas within the intranasal and/or intraoral areas, as well as epistaxis, which is an acute hemorrhage from the nostril, nasal cavity, or nasopharynx. More extensive symptoms of rhinocerebral mucormycosis include ophthalmia and cranial nerve involvement.
Altered immunity in DM and mucormycosis
There are several different aspects of DM that create an ideal environment for Mucorales fungi. First and foremost, patients with DM often exhibit impaired innate and adaptive immunity, which increases their susceptibility to any type of infection, particularly mucormycosis, as this infection is rarely seen in non-immunocompromised hosts.
Upon exposure to Mucorales spores, a competent immune system will send macrophages to engulf spores and prevent their germination. Comparatively, DM patients often have altered phagocytic pathways, thus rendering macrophages unable to phagocytize these spores. As a result, the free spores swell and form buds throughout the blood vessels of the respiratory tract.
Although polymorphonuclear (PMN) cells are recruited to these areas, these cells often exhibit an impaired function in DM patients, which limits their ability to prevent the proliferation of Mucorales. As a result, the fungal spores are able to extensively invade tissues and large blood vessels.
The role of iron and pH
In addition to the altered immune system in DM patients that allows for the proliferation of Mucorales fungi, both the iron and pH levels of DM patients can also contribute to the development of mucormycosis. When cultured in vitro, the R. oryzae Mucorales species cannot survive in human serum due to the sequestration of iron by iron proteins. Comparatively, when present in iron-limited environments, the high-affinity iron permease allows R. oryzae to acquire iron and thrive in these environments.
When the pH of human serum is reduced, which often occurs in ketoacidosis, R. oryzae can disrupt the iron-binding capacity of transferrin. This disrupted function in transferrin, therefore, allows for free iron to be released into the serum, which can be readily used by the Mucorales spore to thrive in these environments.
Epidemiology of DM and mucormycosis
In 2014, it was estimated by the World Health Organization (WHO) that DM affected about 422 million people worldwide. As the prevalence of DM continues to rise in countries around the world, the WHO anticipates that up to 700 million adults worldwide will have DM by the year 2045.
Although the risk factors for DM remain similar between both developed and developing countries, the DM prevalence in developing nations like India is often highest among educated individuals living in urban areas, as compared to those who are uneducated, poor, and/or residing in rural areas. Mucormycosis is most commonly seen in patients with uncontrolled DM, which has a fatality rate ranging from 32% to as high as 57%.
Diagnosis and treatment
Both mucormycosis and aspergillosis are fungal infections that share similar symptoms; therefore, the differential diagnosis of these conditions is essential to ensure that the appropriate treatment is initiated immediately. Some of the different methods that can be used to establish a mucormycosis diagnosis include:
- Presence of comorbidities, particularly DM
- Radiological signs that are compatible with mucormycosis
- Tissue biopsy for microbiological analysis
Once the diagnosis of mucormycosis has been confirmed, several different antifungal drugs can be used that have shown promising results in the treatment of mucormycosis. These several potential antifungal drug combinations. It should be noted, however, that most common antifungals have no activity against Mucorales.
In addition to pharmacological treatment, surgical debridement of necrotic tissue can also be used to leave living tissue as margins. This then allows for antifungal treatments to be locally delivered to infected areas.
References:
- Steinbrink, J. M., & Micheli, M. H. (2021). Mucormycosis. Infectious Disease Clinics of North America 35(2); 435-452. doi:10.1016/j.idc.2021.03.009.
- Al Hassan, F., Aljahli, M., Molani, F., & Almomen, A. (2020). Rhino-orbito-cerebral mucormycosis in patients with uncontrolled diabetes: A case series. International Journal of Surgery Case Reports 73; 324-327. doi:10.1016/j.ijscr.2020.07.011.
- Diabetes statistics 2021 [Online]. Available from: https://www.singlecare.com/blog/news/diabetes-statistics/.
- Rammaert, B., Lanternier, f., Poiree, S., et al., (2012). Diabetes and mucormycosis: A complex interplay. Diabetes & Metabolism 38(3); 193-204. doi:10.1016/j.diabet.2012.01.002.
Last Updated: Jul 12, 2021