Babesiosis is an emerging, zoonotic, tick-borne disease caused by intraerythrocytic protozoan parasites of the genus Babesia, which are transmitted by hard-bodied (Ixodes) ticks. Several different species are known to cause disease in humans, most notably Babesia microti, Babesia divergens and Babesia duncani.
Babesia infection may be completely asymptomatic or may present with illness. The severity of that illness may range from mild to fulminant and sometimes even results in death. Diagnosis should therefore involve a complete descriptive history that includes any clinical manifestations, travel history to endemic areas, tick bite exposure, splenectomy and recent blood transfusion.
Since symptoms and signs of the disease can be relatively non-specific, laboratory testing is essential to establishing a correct diagnosis. The primary diagnostic method is microscopic detection of parasites on blood film examination, although the use of polymerase chain reaction (PCR) is increasing and serodiagnosis can be useful.
Babesiosis - Monsters Inside Me Ep7
Microscopy Detection Methods
The examination of thin blood smears to detect parasites within erythrocytes is the most commonly used technique for diagnosing infections with Babesia microti in the United States (US) and Babesia divergens in Europe. After adequate staining of peripheral blood smears with Giemsa or Wright’s stain, the Babesia parasites can be seen within erythrocytes as darkly-stained ring shapes with pale blue cytoplasm.
It is necessary to examine multiple smears, since, during the early stage of disease (when people tend to seek medical advice,) only a few red blood cells may be infected. Among individuals with healthy immune systems, the extent of parasitemia is rarely more than 5% but can be up to 85% in asplenic people. Furthermore, the duration of parasitemia that is detectable on blood smears varies from person to person, ranging from three weeks to twelve weeks.
There are certain points to consider regarding such blood smear analyses. The ring forms seen within red blood cells can vary significantly and may be mistaken for Plasmodium falciparum (a parasite that causes malaria), although the absence of the hemozoin pigment should point to Babesia parasites. Indeed, cases have been described in scientific literature where patients have been misdiagnosed with malaria, which may result in misguided treatment choices and pose a serious risk to the patient.
Generally, blood smear analysis is a rather subjective process, which inevitably depends on the observer’s experience and the time dedicated to smear examination. The need to differentiate babesial morphology and the likelihood of low-level parasitemia may lead to inaccurate diagnoses, which is why diagnostic approaches are constantly being refined.
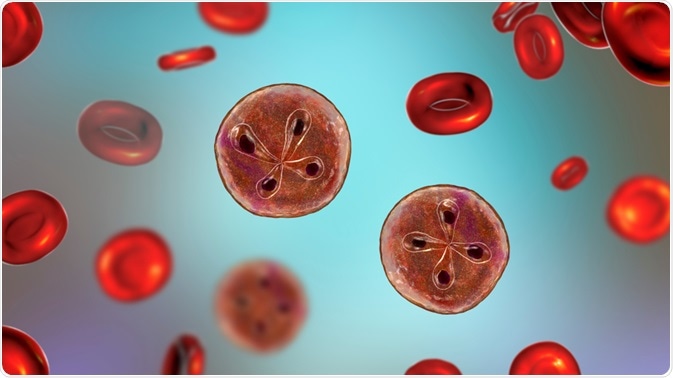 Babesia, the causative agent of babesiosis, parasites inside red blood cells. Image Credit: Kateryna Kon / Shutterstock.com
Babesia, the causative agent of babesiosis, parasites inside red blood cells. Image Credit: Kateryna Kon / Shutterstock.com
Serologic Methods
The indirect immunofluorescence assay (IFA) is a commonly used, sensitive and specific serologic test used to diagnose human babesiosis. The cut-off titer for a positive test result varies between laboratories, although higher titers (1:128 to 1:256) are linked to improved diagnostic specificity.
In the case of Babesia microti infection, antibodies are generally detectable when patients are initially diagnosed, whereas serological diagnosis in the case of Babesia divergens infection is not usually possible due to the infection being too serious or severe since the antibodies are only identifiable 7 to 10 days following the onset of hemoglobinuria.
A potential drawback to serologic testing is the possibility of cross-reactivity due to the presence of other protozoan parasites. This would generate false-positive results. The presence of connective tissue disorders such as rheumatoid arthritis, for example, may also result in a false-positive, whereas a false-negative result may be generated in the case of an immunosuppressed patient.
Molecular Methods
Adequate detection of mild babesiosis infection often entails more sensitive methods than those so far discussed. The development of more sensitive techniques based on PCR has made it possible to diagnose and monitor even mild cases of infection.
In the case of Babesia microti infection and Babesia divergens infection, PCR-based detection assays usually involve the amplification of DNA sequences that are highly conserved and comparison of the resulting fragments with known sequences stored in a database. This enables accurate identification of the infecting parasite.
References
Further Reading
Last Updated: Feb 4, 2021