Skip to:
Stem cell therapies are being sold aggressively for a multitude of health disorders, including arthritis. These are part of a growing new specialty called regenerative medicine, which is aimed at helping the body to replace injured and dead parts naturally, using the body’s own cells.
Arthritis is a degenerative or inflammatory condition of the joint that involves damage to the cartilage that shields the ends of the bones that take part in the joint.

Image Credit: one photo / Shutterstock
Among the different types of arthritis, osteoarthritis is the most common type, affecting about 130 million people worldwide. Stem cells are now marketed as the wonder therapy for arthritis, with hype promising relief from pain, new cartilage growth to replace damaged cartilage, and restoration of joint function.
What are stem cells?
Stem cells are undifferentiated cells, which can proliferate to keep their numbers stable or turn into almost any other type of human cell. This has led to their being viewed as potential wonder therapies for any condition in which dead or worn-out tissue is to be replaced. Moreover, they release signaling molecules that encourage growth and wound healing by mature cells.
There are different sources of stem cells, such as:
- embryonic stem cells derived from the early embryo, making it an ethically contentious issue
- adult stem cells found in small numbers in bone marrow (1 in 20,000 cells) or in fat pads (1 in 2,000), which can give rise to different types of cells
- induced pluripotent stem cells which are formed by genetically reprogramming adult cells into stem cells that closely resemble embryonic stem cells
- perinatal stem cells derived from other fetal tissues such as the amniotic fluid or the umbilical cord
How are stem cells useful in arthritis?
Stem cells are being tried as experimental treatments to help regrow cartilage. Mesenchymal stem cells (MSCs), obtained from umbilical cord blood, can travel to injury sites or inflamed parts of the body and release several different regenerative factors such as vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), and platelet-derived growth factor (PDGF).
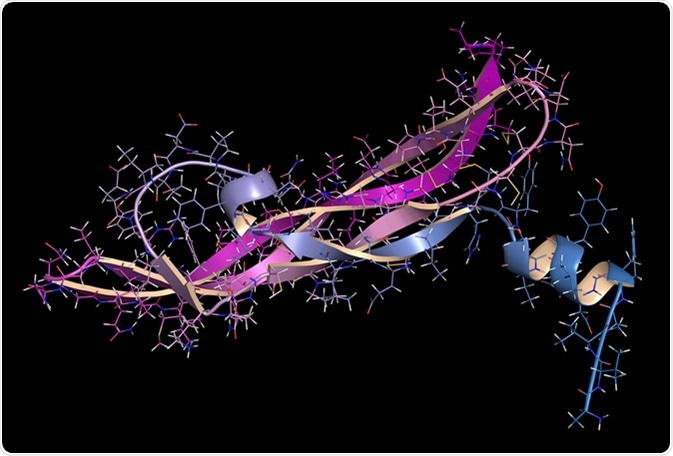
Vascular endothelial growth factor A (VEGF A) protein molecule. 3D rendering. Image Credit: StudioMolekuul / Shutterstock
These can enhance the growth of cartilage and supporting tissue, thus improving tissue repair. In addition, they also have other more subtle effects. For instance, they can reduce the intensity of inflammation as well as prevent a hyperactive immune response.
Anti-inflammatory effects of stem cells
How does this happen? For one, MSCs oppose the actions of several inflammatory molecules, and enhance the expression of TNF-α stimulated gene/protein 6 (TSG-6), which is a protein with multiple anti-inflammatory functions. This reduces macrophage inflammatory signaling, and so tones down the proinflammatory cascade.
In yet another mechanism, MSCs exposed to inflammatory molecules such as lipopolysaccharide, TNF-α, or nitric oxide, released from damaged tissues provide negative feedback by releasing prostaglandin E2 (PGE2). This causes a proinflammatory to anti-inflammatory macrophage phenotype shift. Yet more mechanisms may be found, perhaps involving proteins such as stanniocalcin-1, that oppose the damage caused by reactive oxygen species (ROS).
When cartilage cells are cultured along with stem cells, they grow better and the extracellular matrix (ECM) they build around themselves by secretion is also significantly more stable and similar to that found in living cartilage itself.
On the basis of current knowledge, it appears that infusing umbilical cord MSCs are associated with the greatest degree of improvement, at least in rheumatoid arthritis. However, most stem cell therapies offered today use fat or bone marrow injections, which are not the best forms of stem cells in this condition, since the stem cells make up only a small percentage of the total number of cells injected
Lack of evidence of efficacy in arthritis
A couple of early stem cell studies have shown limited success in cartilage or bone regrowth, which is the only outcome that could potentially cure arthritis.
Stem cells seem to be ideal for replacement of damaged joint tissue. However, this concept can become reality only after a lot of hard work. For one thing, these cells behave differently in vivo and in vitro, so that laboratory experiments may not predict their actual behavior in the body.
Anecdotal reports of stem cell therapy leading to improvement are of less value when compared with rigorously reviewed evidence.
A 2016 systematic review in the Journal of Bone and Joint Surgery failed to show more than placebo-size effects of stem cell therapy in osteoarthritis. This was echoed by another review in 2017, in the BMJ, which said, “In the absence of high-level evidence, we do not recommend stem cell therapy for KOA [knee osteoarthritis].”
Even if stem cells do produce an actual physiological improvement due to their characteristic functions, nobody knows exactly how far this will be sustainable. It is difficult to ensure the stem cells differentiate into cartilage producing cells and remain so, rather than transforming back into undifferentiated cells or into other types of mature cells. Also, it is difficult to ensure they blend with the original joint tissue without evoking an immune reaction. Thirdly, it is a challenge to reproduce the natural strength of joint cartilage with these cells.
Expensive placebos?
Some prominent hospitals claim up to 70% of patients have at least some pain relief, based on available literature rather than their own experience. However, rigorous trials show that there is no clinical difference or anatomical difference between joints treated by saline injections or bone marrow stem cell injections – except for the far higher cost of the latter. This makes it more difficult to disentangle the placebo effect, or pain relief caused by the injection of a foreign substance into the vicinity of the injured joint, from an actual stem-cell induced therapeutic effect.
Though physicians offering stem cell therapy in arthritis claim correctly that they are operating within legal limits, the fact remains that for many, this is an opportunity to peddle a lucrative but apparently unproven, and in many cases unproductive, form of treatment. In the words of bioethicist Leigh Turner, these injections are “expensive placebos.”
As Scott Gottlieb, former FDA commissioner, says, “There’s economic harm here, where products are being promoted that aren’t providing any proven benefits and where patients are paying out-of-pocket.”
Current status of stem cell therapy
No stem cell therapy has received approval from the US Food and Drug Administration (FDA), which is still monitoring the ongoing trials. Stem cells extracted from a patient’s body may be used for that patient only, without any significant processing or modification, without the need for FDA approval. In arthritis, stem cells can be given as injections in addition to standard orthopedic treatment, at best, to help relieve pain and to improve the patient’s quality of life.
Adult stem cells are difficult to isolate or generate in large amounts with current technology. Their potential to differentiate into other types of cells than the tissue of origin is uncertain.
The long-term efficacy and safety of these therapies remains to be proven. Cells in culture show signs of aging, lose their ability to differentiate, and even look different. The use of certain embryonic or induced pluripotent stem cells may potentially cause tumor growth, which means much work remains to be done. Viruses and prions may also be spread via such cells.
Secondly, legality doesn’t mean clinical utility, an issue underlined by several bioethical researchers. Thirdly, many factors influence the behavior of stem cells in vivo, which are only being discovered currently. These factors will play an important role in how, by which route, at what dosage, and with what cofactors, these cells should be administered.
While clinical trials using ethically derived stem cells are to be encouraged unreservedly, to determine the boundaries of utility of this regenerative therapy, it is a matter of concern that stem cell therapy is being unqualifiedly touted as an effective treatment for arthritis.
Sources
- Preparing regenerative therapies for clinical application: proposals for responsible translation. Shane A. Shapiro, Cambray G. Smith, Jennifer R. Arthurs & Zubin Master. Regenerative Medicine Vol. 14, No. 2. https://doi.org/10.2217/rme-2018-0163. https://www.futuremedicine.com/doi/10.2217/rme-2018-0163
- Mayoclinic.org. (2018). Case study: Use of platelet-rich plasma and bone marrow aspirate concentrate injections to treat knee osteoarthritis. www.mayoclinic.org/.../mcc-20422665
- Shane, A. et al., (2018). Quantitative T2 MRI mapping and 12-month follow-up in a randomized, blinded, placebo controlled trial of bone marrow aspiration and concentration for osteoarthritis of the knees. Shane A. Shapiro, Jennifer R. Arthurs, Michael G. Heckman, Joseph M. Bestic, Shari E. Kazmerchak, Nancy N. Diehl, Abba C. Zubair, and Mary I. O’Connor. Cartilage Volume: 10 issue: 4, page(s): 432-443. https://doi.org/10.1177%2F1947603518796142. https://journals.sagepub.com/doi/abs/10.1177/1947603518796142
- Szabo, L. (2019). Elite hospitals plunge into unproven stem cell treatments. khn.org/.../
- Intra-articular cellular therapy for osteoarthritis and focal cartilage defects of the knee: a systematic review of the literature and study quality analysis. Chahla J., Piuzzi N. S., Mitchell J. J., Dean C. S., Pascual-Garrido C., LaPrade R. F., and Muschler G. F. Journal of Bone and Joint Surgery 2016 Sep 21;98(18):1511-21. doi: 10.2106/JBJS.15.01495. https://www.ncbi.nlm.nih.gov/pubmed/27655978
- Stem cell injections in knee osteoarthritis: a systematic review of the literature. Haiko I. M. F. L. Pas, Marinus Winters, Hidde J. Haisma, Martinus J. J. Koenis, Johannes L. Tol, and Maarten H Moen. BMJ Volume 51, Issue 15. http://dx.doi.org/10.1136/bjsports-2016-096793. https://bjsm.bmj.com/content/51/15/1125
- Mayoclinic.org. (2019). Stem cells: What they are and what they do. www.mayoclinic.org/.../art-20048117
- Mesenchymal stem/stromal cells (MSCs): role as guardians of inflammation. Prockop D. J., Oh J. Y. Molecular Therapy 2012 Jan;20(1):14-20. doi: 10.1038/mt.2011.211. https://www.ncbi.nlm.nih.gov/pubmed/22008910/
- The pros and cons of mesenchymal stem cell-based therapies. Aleksandra Musiał-Wysocka, Marta Kot, and Marcin Majka. Cell Transplant. 2019 Jul; 28(7): 801–812. doi: 10.1177/0963689719837897. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6719501/
Further Reading
Last Updated: Feb 11, 2020