The microbiome consists of about 100 trillion microbes (microbiota) and their genomes. These are made of bacteriophage, fungi, bacteria, protozoa (single-cell eukaryotes), and viruses in the human body. They play an important role in health maintenance systems of the immune system, as well as in drugs and foreign substances (xenobiotics) metabolism.
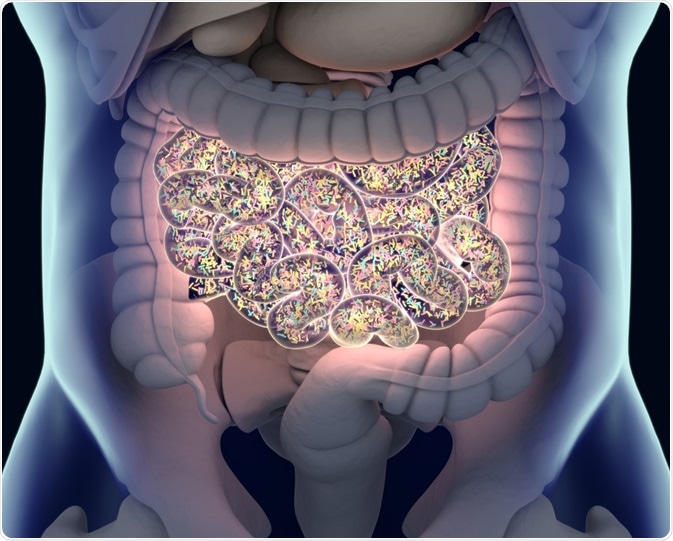 Image Credit: Anatomy Insider / Shutterstock.com
Image Credit: Anatomy Insider / Shutterstock.com
Researchers have discovered that the microbiome influences many human diseases, including cancer. The response of the microbiome towards cancer therapy becomes more evident. Therefore, it is suggested that modifying the microbiome could have an impact on the response of cancer treatments.
The onset of cancer, its progression, as well as the outcomes of cancer therapy, depend on the immune system response. Hence, it is important to understand the influence of the microbiome on the human immune response, specifically to immunotherapy. Immunotherapy uses the specificity of the patients´ immune system to treat cancerous tumors.
Now that many molecular cancer-specific antigens have been identified, it is possible to develop specific antigen immunotherapies. During immunotherapy, antigen-specific T-cells are treated ex-vivo (out of the body) and then injected back into the patients. Vaccination is another type of immunotherapy, in which antigens and T-cells are injected into a person.
Mechanism of the immune system in the gastrointestinal environment
The vast numbers of microbiota within the gut serve a protective role in helping the immune system prevent bacterial and viral infections. In addition to augmenting the localized immune response, microbiota affects immunity at different levels. It is now established that microbiota plays a role in shaping the immune system.
The gut consists of an epithelial cell layer made of intestinal epithelial cells (IECs) and intraepithelial lymphocytes (IELS), which facilitate interactions of the immune system. The lamina propria (connective tissue) of the gastrointestinal tract lies beneath the mucosal layer of the gut. This tissue is the largest component of the body’s immune system.
It contains many immune cells, such as antigen-presenting cells (APCs) and innate lymphoid cells (ILCs). It also hosts CD4+ and CD8+ T cells, which are major immune system players. Furthermore, the gut microbiota impacts both local immunity and systemic immune responses.
Animals used for studying the gastrointestinal environment are germ-free rodents. These animal models do not have any microorganisms and are raised in a germ-free environment. Necessary microorganisms such as gut bacteria are injected during the studies.
Effects of the microbiome upon immunotherapy
Because the microbiome modulates host immunity, it may play an important role in influencing the response and toxicity of different forms of cancer treatment. Different studies have now reported that the microbiome affects response to and toxicity from these therapies. Several types of immunotherapy exist, all of which are likely impacted by the microbiome.
In 2013 Lida et al. observed a reduction of therapeutic response of immunotherapy through a combination of TLR9 antagonist and antibodytointerleukin-10R(IL-10R). In this study, the therapeutic efficacy was reduced when microbiota was absent or changed.
Similar outcomes were reported in a different study by Pitt et al. in 2016, where mice were used to establish the impacts of the microbiome upon CTLA-4 blockade, which is one form of immunotherapy. It was reported that the effects of CTLA-4 blockade depend on specific gut microbiota.
Furthermore, loss of therapeutic efficacy was seen in mice under germ-free conditions. This shows that this type of immunotherapy can be enhanced to work more effectively towards cancer with the facilitation of the microbiome.
A recent study by Zheng et al. in 2019 evaluated the outcomes of checkpoint-blockade immunotherapy targeting programmed cell death protein 1 (PD-1) in patients with hepatocellular carcinoma. The results have shown that patients with higher amounts of gut bacteria responded to the therapy, whereas patients with lower counts of gut bacteria did not respond to the therapy.
Akkermansia muciniphila and ruminococcaceae spp. were two types of bacteria identified playing an important role in patients, where immunotherapy was effective.
Many studies with mice, as well as with patients, provided evidence that gut microbiota potentially enhances the efficacy of CTLA-4 blockade, anti-cell death protein 1 therapy, as well as other types of immunotherapies. The outcomes of the immunotherapy almost always change due to the microbiome.
Although these advances are important to understanding cancer immunotherapy, the mechanisms behind these are not yet fully understood, and optimal therapeutic strategies that enhance cancer immunotherapy are yet to be discovered.
Sources
Gopalakrishnan, V. et al.2018. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. https://doi.org/10.1016/j.ccell.2018.03.015.
Lida, N. et al., 2013. Commensal bacteria control cancer response to therapy by modulating the tumor microenvironment. https://www.ncbi.nlm.nih.gov/pubmed/24264989.
Palucka, K. and Banchereau, J. 2012. Cancer immunotherapy via dendritic cells. https://www.nature.com/articles/nrc3258.
Paulos, C.M. et al., 2007. Toll-like Receptors in Tumor Immunotherapy. https://clincancerres.aacrjournals.org/content/13/18/5280.short.
Pitt J. M. et al. 2016. Fine-Tuning Cancer Immunotherapy: Optimizing the Gut Microbiome. Cancer Research. cancerres.aacrjournals.org/.../0008-5472.CAN-16-0448.
Zheng Y. et al. 2016. Gut microbiome affects the response to anti-PD-1 immunotherapy in patients with hepatocellular carcinoma. Journal for ImmunoTherapy of Cancer. https://jitc.biomedcentral.com/articles/10.1186/s40425-019-0650-9.
Zitvogel, L. et. al. 2016. The microbiome in cancer immunotherapy: Diagnostic tools and therapeutic strategies. https://science.sciencemag.org/content/359/6382/1366.
Further Reading
Last Updated: Nov 7, 2019