The power of EEG
Elevating patient care with EEG
Streamlining workflows with advanced EEG systems
Investing in the future of neurology
References
Further reading
The power of EEG
Electroencephalogram (EEG) is a method used to measure and visualize spontaneous electrical activity within the brain. Electrical impulses are the main form of signaling found within the brain; therefore, measuring this activity can provide invaluable insights into the state of brain activity in both scientific research and the clinic.
EEGs are generated by attaching small metal discs called electrodes to specific points of the scalp. The electrodes capture the electrical activity of neurons in the cortex, creating a small electrical field due to neuronal activity.1 These electrodes are easy to prepare and attach and are noninvasive, making their use ideal in the clinic.

Image Credit: YAKOBCHUK VIACHESLAV/Shutterstock.com
Non-invasive techniques are assessment methods that require no surgery to complete. This style of test benefits clinics because invasive tests require fully sterile environments and are often accompanied by surgical wounds, which require care. Non-invasive tests like EEGs also require less preparation because they do not require anesthesia and often need less staff to complete them.
Elevating patient care with EEG
Due to the diverse benefits of EEGs in clinical applications, EEG is a key component in the diagnosis and monitoring of multiple conditions. One condition in EEGs has proven invaluable in epilepsy. Epilepsy is a disorder characterized by seizures arising due to aberrant brain activity. 2
Seizures, however, may be hard to catch, as they may occur when a trained professional isn't present or at night. Because seizures arise due to aberrant brain activity, they can be detected using EEG. EEGs leverage the appearance of interictal epileptiform discharges (IED), which appear between seizures. 3
EEGs can be used to visualize the patterns generated by the IED, and these patterns are well-characterized, allowing clinicians to diagnose individuals accurately. (Rosenow et al., 2015) EEGs are also highly specific to diagnosing epilepsy, detecting between 60-90% of IED in patients by the fourth EEG, compared with non-epileptic patients at 0.5-2.5%, the chances of a false diagnosis are very low. 4
Sleep disorders may also be diagnosed using EEGs. Sleep disorder is a term used to describe a variety of disorders that cause abnormal or affected sleep, such as narcolepsy, sleep apnea, and insomnia.
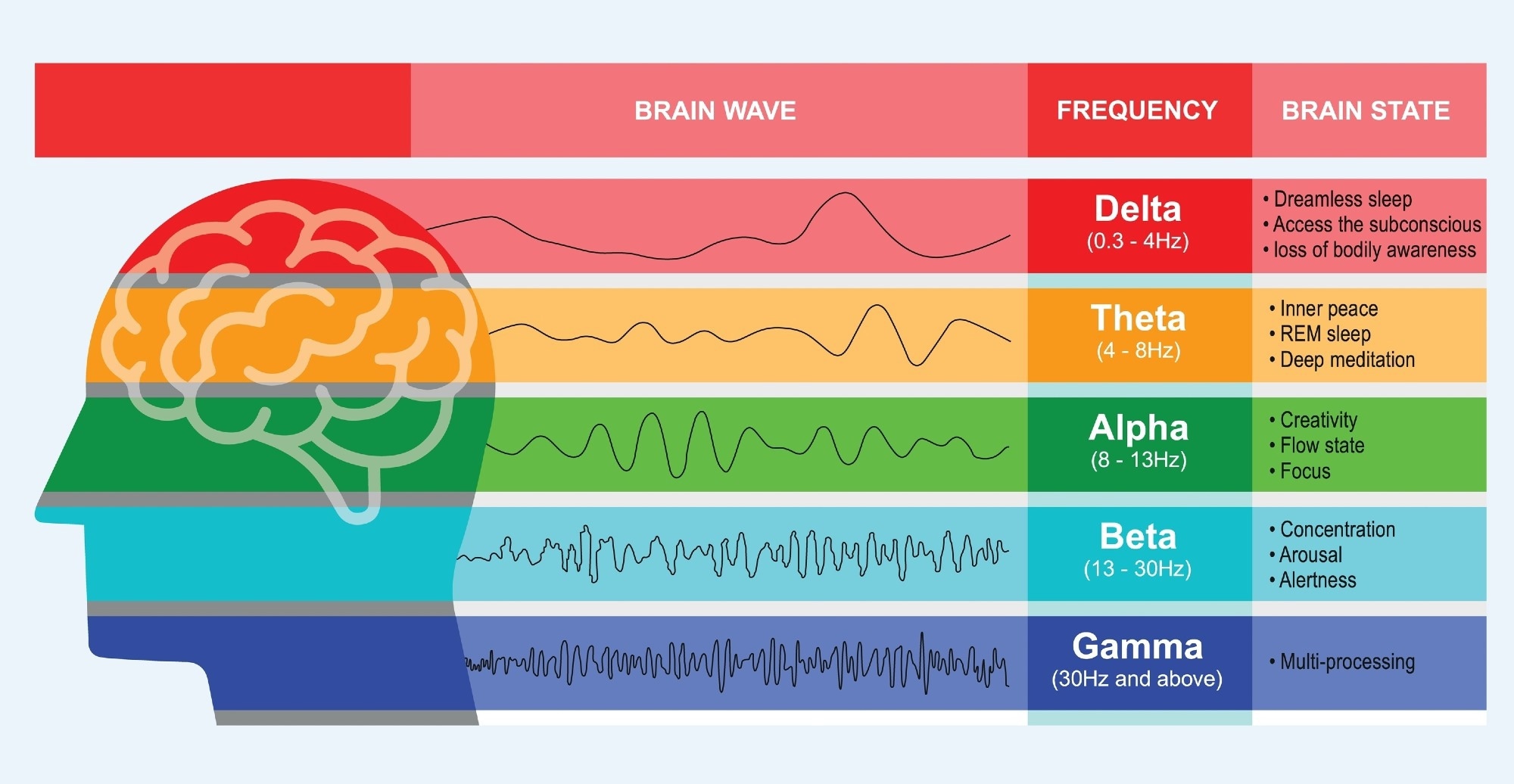
Brain wave function EEG chart. Image Credit: Vallabh Soni/Shutterstock.com
When assessing such disorders, a patient undergoes an EEG during a night's sleep to assess sleep quality through brain activity. In studies used to assess EEGs in diagnosing sleep apnea, EEG has proved invaluable for electrophysiological monitoring. 5
Outside of disease and disorder diagnosis, EEG can also be used as a tool to monitor the effectiveness of anesthesia in patients. It is thought that anesthetics induce brain waves that either alter or disrupt the normal brain wave patterns. Therefore, EEGs can be used to visualize and measure these aberrant brain waves, providing insight into how sedated a patient is. 6
Streamlining workflows with advanced EEG systems
Advancements in EEG technology
Due to its power in a variety of disorder diagnoses and interventions, EEG technology is rapidly advancing, streamlining the workflow for operators and clinicians. Digitizing EEGs has been a huge step, both for the collection and interpretation of results.
Analogue EEGs (the last generation of this technology) used paper to graph the test results. Instead, digital EEGs map these results electronically, such as directly onto a computer or another form of physical digital storage.
The large data output produced from EEGs meant that storage of results on paper could take up huge amounts of space. Digitizing this data, therefore, saves both space and resources, lowering long-term costs. Digital EEGs also benefit from being able to alter the parameters of the visualized output and automatic event detection. This ability to filter and set automatic detection improves the accuracy of EEG in clinical usage. 7
Innovations for long-term monitoring
While clinics use EEGs for a short period (typically less than an hour), diagnosis sometimes requires measurements to be taken over a larger time frame. This can pose challenges in traditional EEG systems, which are bulky and often attached directly to a computer, meaning longer recordings are unviable.
Ambulatory EEGs utilize a mobile recording device that the EEG electrodes can plug into. This allows a patient to retain their mobility and carry on with many day-to-day activities. Ambulatory EEGs have been shown to be massively beneficial in epilepsy diagnosis, as the prolonged period it is used over captures more IEDs and ictal events. 8
Streamlining EEG analysis with cloud-based systems
Traditionally, EEG data analysis has been completed by professionals with the required training to understand the complex and large data output of the technique. These large datasets typically slow down patient diagnosis due to the time taken to analyze and interpret such data. However, recent advances in technology have slim-lined this process massively.
Cloud-based EEGs leverage cloud computing (a system that uses on-demand computing services through the internet) to streamline the storage and interpretation of such data. This allows the large datasets produced by EEGs to be stored on non-local servers, saving valuable space.
A 2021 study found that through the incorporation of an integrated program with cloud computing, EEG analysis was greatly improved in speed, allowing for more neurophysiologic examinations to be performed. 9
This cloud-based approach also offers huge value in terms of data access. Physicians may access data in different locations, such as between offices and at home. Furthermore, software has been developed that allows for the live monitoring of EEG results remotely. This means a physician does not have to be physically present when the EEG is administered, offering huge flexibility.
Investing in the future of neurology
EEGs are invaluable in the detection and monitoring of a range of disorders. Increasing the accuracy and speed at which these disorders are identified is critical for providing early care, massively benefitting patients in long-term prognosis.
Due to their noninvasive nature, EEGs are easy to set up, and through advances in EEG technology and workflows, they are becoming increasingly easy to interpret outputs. The ease of use of readily available online resources alongside the relatively low cost of equipment and consumables means clinical adoption is easy and efficient, providing huge returns on investment in the system.
References
- Rayi, A., and Murr, N. I. (2024) Electroencephalogram. https://pubmed.ncbi.nlm.nih.gov/33085442/
- Manford, M. (2017) Recent advances in epilepsy. Journal of Neurology 264(8): 1811–1824. https://pubmed.ncbi.nlm.nih.gov/28120042/
- Smith, E. H., Liou, J., Merricks, E. M., Davis, T., Thomson, K., Greger, B., House, P., Emerson, R. G., Goodman, R., McKhann, G. M., Sheth, S., Schevon, C., and Rolston, J. D. (2022) Human interictal epileptiform discharges are bidirectional traveling waves echoing ictal discharges. eLife 11. https://elifesciences.org/articles/73541
- Maurer JT. Early diagnosis of sleep related breathing disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2008;7:Doc03. Epub 2010 Oct 7. PMID: 22073090; PMCID: PMC3199834. https://pmc.ncbi.nlm.nih.gov/articles/PMC3199834/
- Patrick L. Purdon, Aaron Sampson, Kara J. Pavone, Emery N. Brown; Clinical Electroencephalography for Anesthesiologists: Part I: Background and Basic Signatures. Anesthesiology 2015; 123:937–960 doi: https://doi.org/10.1097/ALN.0000000000000841
- Van Cott, A., & Brenner, R. P. (1998). Technical advantages of digital EEG. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society, 15(6), 464–475. https://doi.org/10.1097/00004691-199811000-00003
- Udaya Seneviratne, Wendyl Jude D'Souza, Chapter 10 - Ambulatory EEG, Editor(s): Kerry H. Levin, Patrick Chauvel, Handbook of Clinical Neurology, Elsevier, Volume 160, 2019, Pages 161-170, ISSN 0072-9752, ISBN 9780444640321,https://doi.org/10.1016/B978-0-444-64032-1.00010-2.
- Bertuccio, S., Tardiolo, G., Giambò, F. M., Giuffrè, G., Muratore, R., Settimo, C., Raffa, A., Rigano, S., Bramanti, A., Muscarà, N., & De Cola, M. C. (2021). ReportFlow: an application for EEG visualization and reporting using cloud platform. BMC medical informatics and decision making, 21(1), 7. https://doi.org/10.1186/s12911-020-01369-7
Further Reading
Last Updated: Nov 27, 2024