Epididymitis is usually diagnosed using information from a physical exam of the individual, complemented by sexually transmitted infection (STI) screening and other tests. It is important that a differential diagnosis is made to exclude other conditions, such as testicular torsion, that require immediate treatment to prevent severe complications.
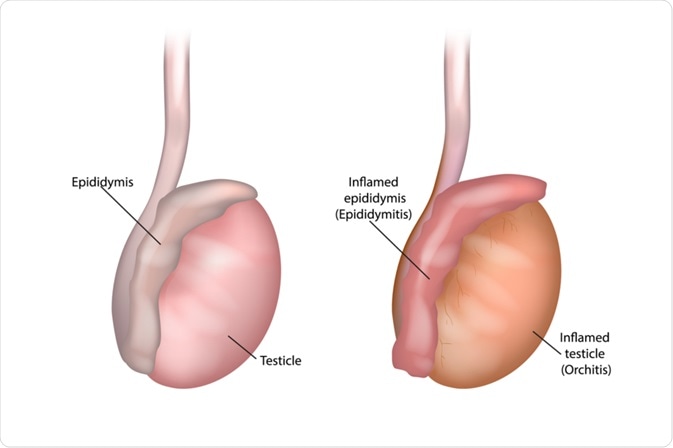
Image Credit: Sakurra / Shutterstock.com
Medical history
Patients with epididymitis typically present with scrotal pain and swelling, usually but not always localized to one side, that gradually develops over a few days.
Patients may report symptoms such as pain on urination or an increased frequency and urgency of urination. Additionally, there may be some discharge from the penis, and pain during sexual intercourse is also often reported. Fever is present in about 1 in 4 patients with acute epididymitis but is more common in children with the condition or for patients with chronic symptoms.
Physical exam
A physical exam is usually the first step in the diagnostic process of epididymitis when a patient presents with symptoms that may be indicative of the condition.
The key signs that will be evident in the physical exam may include:
- Tender red lump on the affected side of the scrotum
- Inflammation of the testicles
- Enlarged lymph nodes in the groin
- Discharge from the penis
A rectal examination is also often carried out to identify an enlarged or tender prostate that may be responsible for causing the symptoms.
STI screening
As STIs are the most common cause of epididymitis in young men, a screening test is often indicated to check for the presence of an infection. This is particularly important if the individual has recently engaged in sexual activities without using a condom.
STI screening involves the insertion of a narrow swab into the urethra of the penis to take a sample of the discharge, which can be analyzed in a laboratory for the most common causative bacteria, as well as for the presence of gonorrhea and/or chlamydia.
Other tests
There are several other tests that may be useful to help in the diagnosis of epididymitis, which include:
- Urinalysis and culture
- Complete blood count (CBC) testing
- Doppler ultrasound imaging
- Testicular scan with nuclear medicine scan
The ultrasound imaging test is particularly useful in the differential diagnosis to rule out other conditions that require different treatments.
Differential diagnosis
Testicular torsion is a condition involving reduced blood supply to testicles and is associated with similar symptoms to epididymitis. It is important to make a differential diagnosis, as testicular torsion requires immediate medical attention with a surgical procedure.
The symptoms tend to present suddenly in testicular torsion, whereas the symptoms will gradually develop over a few days in epididymitis. Doppler ultrasound imaging tests are also useful to examine the blood flow to the testicles and recognize the reduced flow characteristic of testicular torsion.
Other conditions with symptoms that may be confused with epididymitis include:
- Hydrocele
- Non-seminomatous testicular tumors
- Orchitis
- Spermatocele
- Testicular seminoma
Classification: acute or chronic
Epididymitis can be classified as acute or chronic, depending on the duration of symptoms.
Acute epididymitis lasts for less than six weeks and is marked by symptoms of pain, swelling, and inflammation of the scrotum and pelvic region.
Chronic epididymitis involves symptoms that continue for more than six weeks, such as pain or discomfort in the scrotum or pelvic region. This type can be further categorized as inflammatory chronic epididymitis, obstructive chronic epididymitis, or chronic epidiymalgia.
References
Further Reading
Last Updated: Dec 21, 2022