Red blood cells (RBCs) contain hemoglobin (Hg) to allow for oxygen to bind to carbon dioxide (CO2). There are three types of Hg in humans, which include embryonic, fetal, and adult Hg.
What is fetal hemoglobin?
Fetal hemoglobin (HbF) is the form of hemoglobin that is dominant during fetal life and is also markedly increased in concentration for several weeks after birth. Its presence was first noted by E. von Korber in 1866, who found that blood from the umbilical cord contained Hg which was not denatured following exposure to strong acids or alkalis, unlike adult Hg.
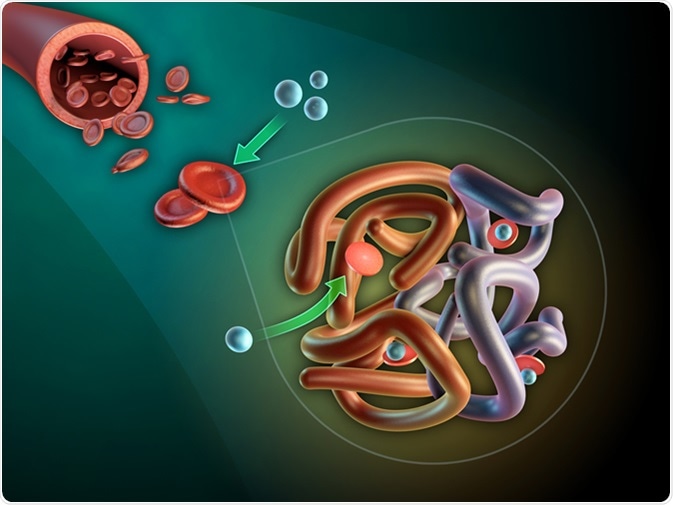
Image Credit: Andrea Danti / Shutterstock
Function of HbF
HbF is a form of Hg that has a stronger oxygen affinity as compared to adult Hg. This greater affinity towards oxygen increases its transport to the fetus within the uterus by capturing oxygen from the placental vasculature, which has much lower oxygen tension than in the lungs. The decline in its production by about 6 months after birth reduces oxygen exchange between the blood vessels and other parts of the body, including the brain.
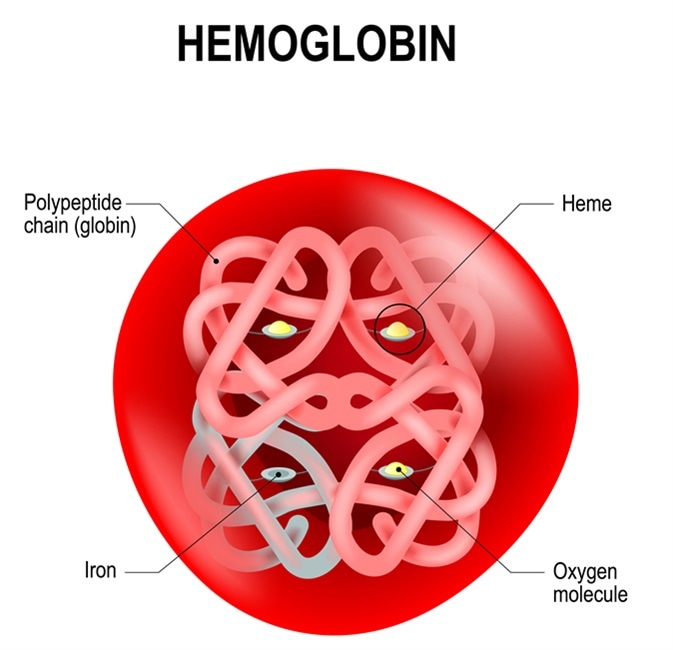
Image Credit: Designua / Shutterstock
Structure of HbF
HbF is present in fetal life; however, its production ceases in the period just after the child is born. Like adult Hg, HbF is made up of four units, of which include two alpha and two gamma units, the latter of which replaces the beta units of adult Hg. The difference between these two Hg forms is in the sequence of 39 amino acids out of the total 146, which is the same for both types.
Indications for HbF testing
An HbF test is required if there is a clinical suspicion of diseases, such as beta-thalassemia, myeloid leukemia, and sickle cell disease, as this variant of Hg is more resistant to sickling and confers survival advantages in the case of thalassemia.
Such conditions may manifest themselves in the form of anemia, with palpitations, chest pain, excessive tiredness, swelling of the feet, and cardiac failure as a result of severe anemia. Again, a family history of such disorders is an indication for HbF testing, as these have a strong genetic basis in most cases.
HbF levels drop by about 10% per fortnight and usually become non-measurable by about six months of postnatal life. The production of HbF is typically reduced to levels of less than 0.6% of an adult’s total hemoglobin.
HbF makes up a sub-population of erythrocytes called 'F-cells.' It has been found that the RBCs of about 85% of adults are comprised of between 0.3% and 4.4% of these specialized cells, showing great variations within the population. This variation in percentage appears to be regulated by genetic factors which are not yet clear. Increased HbF may be due to a rise in the number of F cells and the HbF concentration in existing F cells.
Future research
The importance of HbF also comes from the fact that its natural variants have provided a considerable amount of information on how globin genes are controlled and their synthesis is switched from one form to another.
Current research studies are also being conducted to elucidate which would be the best drugs to increase HbF levels in adults who had low levels of adult Hg or abnormal Hg chains, the latter of which is the case in thalassemia, by switching gene transcription as desired without causing undue toxicity to the patient.
References
Further Reading
Last Updated: May 7, 2021