Conditions similar to fibromyalgia
Fibromyalgia and other related conditions
Conclusion
References
Further reading
Fibromyalgia is a complex syndrome with a wide array of symptoms, including chronic widespread pain, fatigue, sleep disturbances, cognitive dysfunction, and psychological issues. The diagnosis and management of this condition remain challenging due to its multifaceted nature and the evolving understanding of its pathogenesis.1-3
Diagnosing fibromyalgia can be challenging due to the lack of specific biomarkers and the overlap of its symptoms with other conditions.
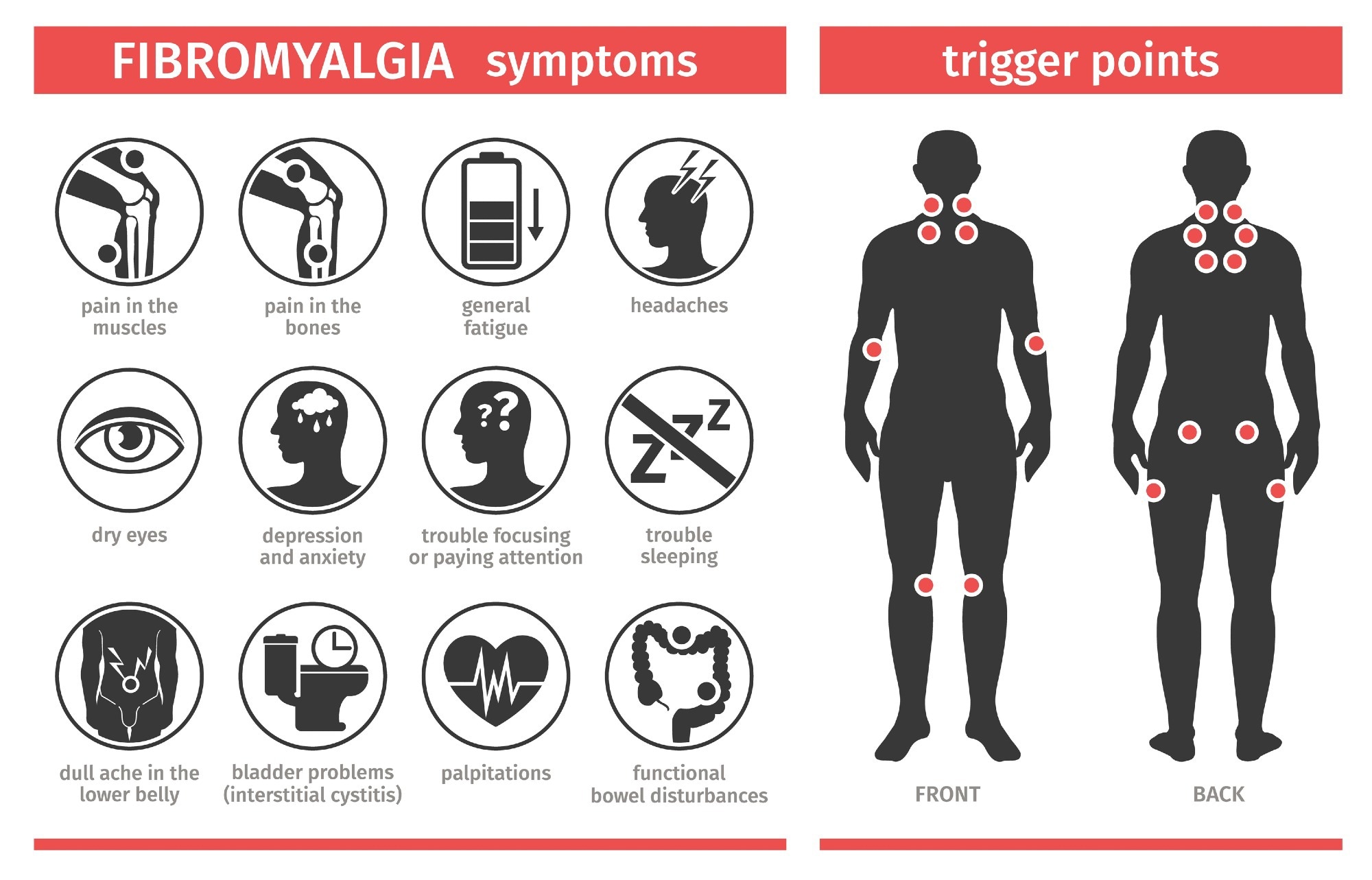 Symptoms and signs of fibromyalgia. Image Credit: Leyasw/Shutterstock.com
Symptoms and signs of fibromyalgia. Image Credit: Leyasw/Shutterstock.com
Conditions similar to fibromyalgia
Hypothyroidism
There is a significant correlation between fibromyalgia and hypothyroidism, with a remarkable overlap in symptoms and a higher prevalence of fibromyalgia among patients with hypothyroidism. In this regard, it has been shown that approximately 40% of patients with hypothyroidism also have fibromyalgia, thereby evidencing a high rate of co-occurrence.4
Both conditions share common symptoms, such as chronic pain, fatigue, and non-restorative sleep, making differential diagnosis challenging. Given these overlapped symptoms, it is recommended that patients with hypothyroidism be evaluated for fibromyalgia and vice versa to ensure comprehensive management4.
Chronic rheumatic diseases
Several studies revealed that fibromyalgia is more prevalent in patients with inflammatory rheumatic diseases compared to the general population,5-7 complicating both diagnosis and treatment. Recognizing and addressing fibromyalgia in these patients is essential for optimal disease management and improving patient outcomes.
The prevalence rates vary across different conditions:
- Rheumatoid Arthritis: 4.9% to 6.6%5-7
- Spondyloarthritis: 11.1% to 12.6%5-7
- Connective tissue diseases such as Sjögren's Syndrome and Systemic Lupus Erythematosus: 11.3% to 13.4%5-7
The American College of Rheumatology (ACR) guidelines established for diagnosing fibromyalgia changed over time:
- 1990 Criteria: Focused on widespread pain and tender points, which are sensitive areas of the body that cause pain when pressed.
- 2010/2011 Criteria: A widespread pain index (WPI) and symptom severity scale (SSS) improved sensitivity and specificity to 86% and 90%, respectively.8,9
- 2016 Revisions: Added a generalized pain criterion to minimize misclassification and combined physician and questionnaire criteria for better accuracy.8
Rheumatic arthritis
It is believed that prolonged exposure to inflammation and pain associated with rheumatoid arthritis can trigger the transition from acute peripheral pain to chronic, centralized pain characteristic of fibromyalgia.

Image Credit: simona pilolla 2/Shutterstock.com
Fibromyalgia increases disease activity, often preventing an adequate response to immunosuppressive treatments10. However, the precise molecular mechanisms linking inflammation to pain amplification remain unclear.
Systemic lupus erythematosus (SLE)
There is a significant association between fibromyalgia and SLE, with fibromyalgia being more prevalent in SLE patients. This coexistence is linked to worse health outcomes and quality of life, with psychiatric symptoms and disease duration being notable contributing factors. The underlying mechanisms may involve common pathways related to pain and distress, such as N-methyl-D-aspartate (NMDA) receptor activity.11-13
Shared symptoms:
- Musculoskeletal pain
- Fatigue
- Stiffness
- Cold sensitivity
- Cognitive difficulties
- Depression
Sjögren’s syndrome (SS)
Patients with fibromyalgia have been found to have a higher risk of developing Sjögren's syndrome. A cohort study suggested that fibromyalgia patients had twice the risk of developing SS compared to those without fibromyalgia, with the risk being particularly high in patients aged 20-49 years14.
Polymyalgia rheumatica (PR)
Both fibromyalgia and PR present with symptoms such as muscle pain and stiffness, which can lead to confusion in diagnosis. PR is characterized by proximal myalgia and chronic inflammation, while fibromyalgia manifests as chronic pain of undetermined etiology.
Despite symptom overlap, PR and fibromyalgia are not the same clinical entities. PR is often considered part of a spectrum of diseases and is better viewed as an extreme of a continuum rather than a separate condition. Fibromyalgia, on the other hand, often may be associated with functional disorders (including depression) without a clear inflammatory component15.
Myofascial pain syndrome
Fibromyalgia and myofascial pain syndrome (MPS) are distinct conditions, with fibromyalgia being characterized by widespread pain and tender points, while myofascial pain syndrome involves localized pain with trigger points and taut muscle bands. However, MPS may potentially evolve into fibromyalgia through deranged myofibroblasts present in connective tissue or fascial armoring.16
Fibromyalgia and other related conditions
Chronic fatigue syndrome (CFS)
While fibromyalgia and CFS are interrelated conditions, they have distinct characteristics. CFS may cause muscle or joint pain, but it's not the main symptom. Moreover, fibromyalgia can cause extreme fatigue, but it's secondary to the pain.
Shared Symptoms:
- Pain
- Fatigue
- Sleep disturbances
- Dizziness
- Cognitive difficulties
- Digestive issues
- Anxiety
- Depression
Diabetes mellitus
There is ongoing debate regarding the exact nature of the relationship between fibromyalgia and type 2 diabetes mellitus (T2DM). While some studies suggest a higher prevalence of fibromyalgia among individuals with T2DM, particularly those with poor glycemic control,17 others have found similar rates of fibromyalgia in T2DM patients compared to the general population.18 Improved blood glucose control may potentially alleviate pain symptoms in T2DM patients with fibromyalgia.18
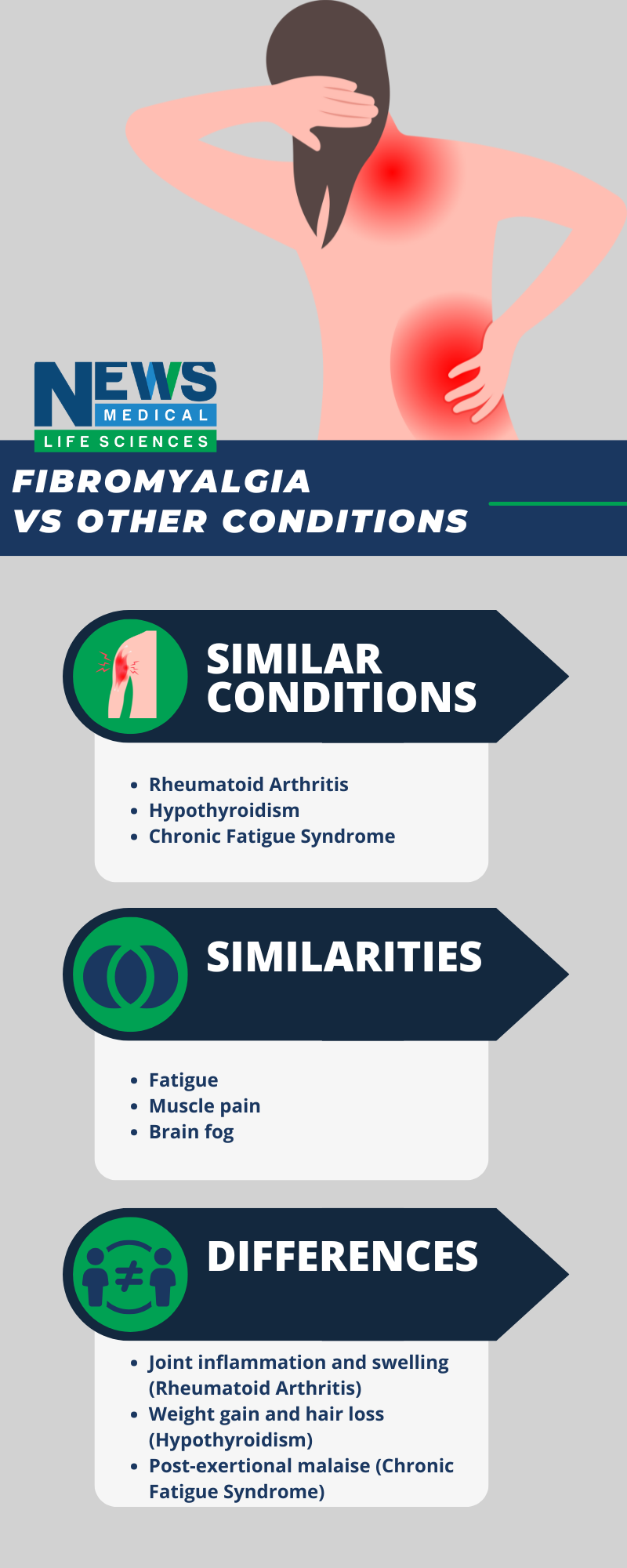
Image Credit: News-Medical.net
Obesity
Obesity is a common comorbidity in patients with fibromyalgia. This condition (obesity) is well-known to be associated with greater pain sensitivity, poorer sleep quality, and reduced physical strength and flexibility.19 Additionally, obesity has also been associated with altered neuroendocrine indices and impaired physical functioning in patients with fibromyalgia.19
Carpal tunnel syndrome (CTS)
Epidemiological data suggests a high prevalence of Carpal tunnel syndrome (CTS) among individuals with fibromyalgia. The most common CTS symptoms in fibromyalgia patients include paresthesia (numbness or tingling) in the hands and sensory-motor deficits. Furthermore, it has been shown a strong correlation between the severity of CTS and functional impairment in patients with fibromyalgia.
Temporomandibular disorders
Fibromyalgia has a high prevalence of temporomandibular disorders, with muscle pain, temporomandibular joint pain, and muscle tenderness on palpation being common symptoms.20
Conclusion
Fibromyalgia often coexists with various other medical conditions. The intricate relationship between this chronic condition and other diseases highlights the multifaceted nature of this disorder.
While the exact mechanisms underlying these associations remain unclear, it is evident that shared pathophysiological pathways, such as inflammation, immune dysfunction, and neurotransmitter imbalances, may contribute to the development and progression of all these conditions.
Further research is needed to elucidate molecular mechanisms and develop targeted therapeutic interventions for fibromyalgia and its comorbidities.
References
- Sarzi-Puttini, P., Giorgi, V., Marotto, D., & Atzeni, F. (2020). Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nature Reviews Rheumatology, 16, 645 - 660. https://doi.org/10.1038/s41584-020-00506-w.
- Smith, H., Harris, R., & Clauw, D. (2011). Fibromyalgia: an afferent processing disorder leading to a complex pain generalized syndrome. Pain physician, 14 2, E217-45.
- Siracusa, R., Paola, R., Cuzzocrea, S., & Impellizzeri, D. (2021). Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. International Journal of Molecular Sciences, 22. https://doi.org/10.3390/ijms22083891.
- Yılmaz, D., Erismis, B., Ustun, E., Koçoğlu, H., & Beş, C. (2021). How Common is Fibromyalgia in Patients with Hypothyroidism?. BOĞAZİÇİ TIP DERGİSİ. https://doi.org/10.21203/rs.3.rs-288062/v1.
- Fan, A., Pereira, B., Tournadre, A., Tatar, Z., Malochet-Guinamand, S., Mathieu, S., Couderc, M., Soubrier, M., & Dubost, J. (2017). Frequency of concomitant fibromyalgia in rheumatic diseases: Monocentric study of 691 patients. Seminars in arthritis and rheumatism, 47 1, 129-132. https://doi.org/10.1016/j.semarthrit.2017.01.005.
- Fan, A., Tournadre, A., Pereira, B., Tatar, Z., Couderc, M., Malochet-Guinamand, S., Sylvain, M., Soubrier, M., & Dubost, J. (2016). AB1008 Prevalence of fibromyalgia in Inflammatory Rheumatic Disease. Single-Center Cross-Sectional Study in 691 Patients. Annals of the Rheumatic Diseases, 75, 1246 - 1246. https://doi.org/10.1136/annrheumdis-2016-eular.1988.
- Haliloglu, S., Çarlıoğlu, A., Akdeniz, D., Karaaslan, Y., & Koşar, A. (2014). Fibromyalgia in patients with other rheumatic diseases: prevalence and relationship with disease activity. Rheumatology International, 34, 1275-1280. https://doi.org/10.1007/s00296-014-2972-8.
- Wolfe, F., Clauw, D., Fitzcharles, M., Goldenberg, D., Häuser, W., Katz, R., Mease, P., Russell, A., Russell, I., & Walitt, B. (2016). 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Seminars in arthritis and rheumatism, 46 3, 319-329. https://doi.org/10.1016/j.semarthrit.2016.08.012.
- Goldenberg, D. (2009). Diagnosis and differential diagnosis of fibromyalgia. The American journal of medicine, 122 12 Suppl, S14-21. https://doi.org/10.1016/j.amjmed.2009.09.007.
- Azevedo, M., Prétat, T., & Hügle, T. (2022). [Assessment of secondary fibromyalgia in patients with rheumatoid arthritis or spondylarthritis]. Revue medicale suisse, 18 773, 477-481 . https://doi.org/10.53738/revmed.2022.18.773.477
- V Torrente-Segarra, T., Carbonell-Abelló, J., Castro-Oreiro, S., & Jm, M. (2010). Association between fibromyalgia and psychiatric disorders in systemic lupus erythematosus. Clinical and experimental rheumatology, 28 6 Suppl 63, S22-6 .
- Park, D., Takahashi, Y., Kang, J., Yim, Y., Kim, J., Lee, J., Lee, K., Lee, J., & Lee, S. (2017). Anti-N-methyl-D-aspartate receptor antibodies are associated with fibromyalgia in patients with systemic lupus erythematosus: a case-control study. Clinical and experimental rheumatology, 35 Suppl 105 3, 54-60.
- Staud, R. (2006). Are patients with systemic lupus erythematosus at increased risk for Fibromyalgia?. Current Rheumatology Reports, 8, 430-435. https://doi.org/10.1007/S11926-006-0037-Z.
- Gau, S., Leong, P., Lin, C., Tsou, H., & Wei, J. (2021). Higher Risk for Sjögren's Syndrome in Patients With Fibromyalgia: A Nationwide Population-Based Cohort Study. Frontiers in Immunology, 12. https://doi.org/10.3389/fimmu.2021.640618.
- Wermelinger, F. (2006). [Polymyalgia rheumatica--fibromyalgia-syndrome: symptoms, syndromes or diseases?]. Therapeutische Umschau. Revue therapeutique, 63 3, 195-200 . https://doi.org/10.1024/0040-5930.63.3.195.
- Plaut, S. (2021). Scoping review and interpretation of myofascial pain/fibromyalgia syndrome: An attempt to assemble a medical puzzle. PLoS ONE, 17. https://doi.org/10.1371/journal.pone.0263087.
- Salman, S., & Abdali, H. (2023). Prevalence of fibromyalgia syndrome among patients with type 2 diabetes mellitus. Rheumatology. https://doi.org/10.1093/rheumatology/kead104.135.
- Tugrul, G., Coskun, C., Sarpel, T., Sert, M., & Nazlıcan, E. (2016). THU0559 Frequency of fibromyalgia Syndrome in Patients with Type 2 Diabetes Mellitus. Annals of the Rheumatic Diseases, 75, 394 - 394. https://doi.org/10.1136/annrheumdis-2016-eular.4254.
- Okifuji, A., Donaldson, G., Barck, L., & Fine, P. (2010). Relationship between fibromyalgia and obesity in pain, function, mood, and sleep. The journal of pain: official journal of the American Pain Society, 11 12, 1329-37. https://doi.org/10.1016/j.jpain.2010.03.006.
- Ayouni, I., Chebbi, R., Hela, Z., & Dhidah, M. (2019). Comorbidity between fibromyalgia and temporomandibular disorders: a systematic review. Oral surgery, oral medicine, oral pathology and oral radiology, 128 1, 33-42. https://doi.org/10.1016/J.OOOO.2019.02.023.
Further Reading
Last Updated: Dec 18, 2024