Gardner syndrome is a genetic disease that comprises the clinical triad of osteomas, polyposis coli, and mesenchymal tumors of the skin and soft tissue.
Incidence and genetics
Gardner syndrome, which is inherited in an autosomal dominant manner, occurs in approximately one in 8,000 people. This condition arises as a result of a mutation on the adenomatous polyposis coli (APC) gene on chromosome 5q21, thereby classifying Gardner syndrome as part of the familial adenomatous polyposis syndromes. All parts of the world are equally affected and there is no gender difference.
About 75% of patients have a family history of Gardner’s syndrome; however, a fourth of all Gardner syndrome patients will exhibit a mutation that arises de novo. The symptoms of Gardner’s syndrome can be developed any time between the ages of two months and 70 years; however, it is more common for symptoms to begin around 10-20 years of age.
Odontomas
Gardner syndrome is often first identified in a dental clinic, as it is associated with odontomas and impacted teeth at multiple sites that can be both permanent and supernumerary. In fact, about 30% of patients with Gardner’s syndrome have one or more dental anomaly.

Image Credit: Rames Khusakul / Shutterstock.com
Maxillofacial involvement is very common in these patients and can involve skin cysts, pigmentation, and various radiographic anomalies. Odontomas also arise in the paranasal sinuses and mandible, and are rarely painful, generally occurring after puberty.
Osteomas
Multiple osteomas also occur in Gardner's. The most common site for these types of tumors is the mandible, specifically at the angle of the jaw and the inferior surface of this bone. Additional osteomas may be present in the skull, paranasal sinuses, and long bones.
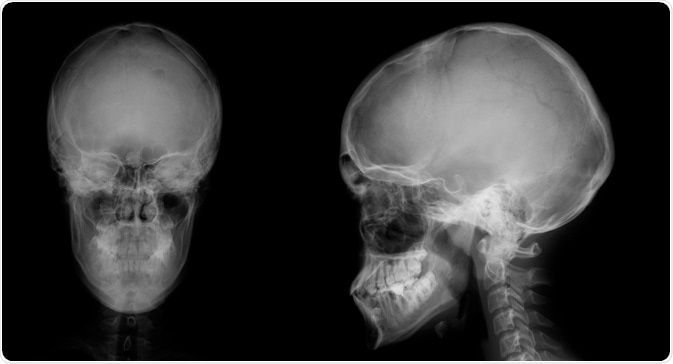
Image Credit: vanzittoo / Shutterstock.com
Osteomas occur early in the course of the disease, typically before colonic polyps become symptomatic or are picked up by radiography. In fact, it is not uncommon for osteomas to develop in Gardner syndrome patients before the condition is even diagnosed. For this reason, the presence of osteomas should arouse curiosity as to the presence of Gardner’s syndrome, as they offer a window of opportunity for early diagnosis and possible prevention of colonic cancer. A number of researchers, therefore, suggest that radiography of the mandible may help to screen for carriers of this condition.
Both osteomas and odontomas may cause the face to become asymmetric. Both sharply-defined radio-opaque lesions as well as fuzzy radio-opaque lesions can be visualized in patients with Gardner's syndrome.
Skin lesions
The most frequently found skin manifestation of Gardner’s syndrome is the epidermoid cyst which occurs in 50-60% of patients. All parts of the body may be affected by these lesions; however, the face, limbs, and scalp are especially targeted.

Image Credit: jaojormami / Shutterstock.com
Desmoid tumors also occur over the abdominal wall, as fibrous tumors with a benign course. Fibrous tumors are notorious for their high recurrence rate and occur in about 9% of patients. Retinal pigment epithelium hypertrophy present at birth is another possible finding.
Polyposis
The most common gastrointestinal presentation of Gardner’s syndrome involves nausea, vomiting, mucous, bloody diarrhea, and abdominal cramps or pain. Additional symptoms that can present in many cases include anemia and, to a lesser extent, symptoms of a bowel obstruction.
Taken together, these symptoms are due to adenomatous polyps of the colon of various types such as tubular, villous, and tubulovillous polyps. These polyps will often carpet the whole colon and rectum when seen on colonoscopy.
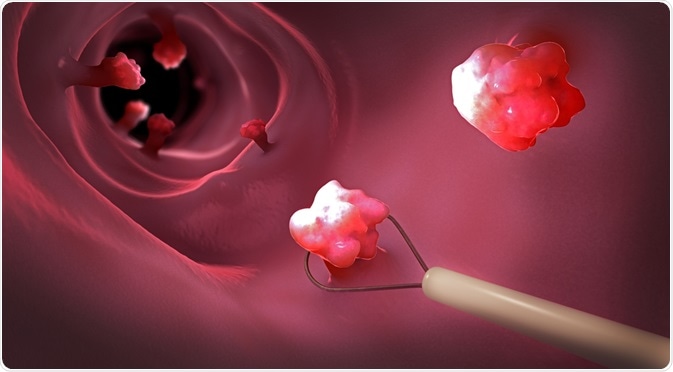
Image Credit: Cristoph Burgstedt / Shutterstock.com
Mostly smaller than 5 mm in size, these polyps can be difficult to detect by imaging. In addition to their presence within the colon, the polyposis of Gardner's syndrome may also cause growths to arise within the mucosa of the stomach or small intestine in up to 12% of cases. Larger polyps may prolapse through the anus or may cause intussusception or obstruction.
The most serious implication of this syndrome is colonic carcinoma, which occurs in about 2 of every 100 cases at presentation and in all patients by the age of 40 unless treated earlier.
References
- Panjwani, S., Bagewadi, A., Keluskar, V., & Arora, S. (2011). Gardner’s Syndrome. Journal of Clinical Imaging Science, 1, 65. http://doi.org/10.4103/2156-7514.92187.
- Basaran, G., & Erkan, M. (2008). One of the Rarest Syndromes in Dentistry: Gardner Syndrome. European Journal of Dentistry, 2, 208–212.
- Ftiadis, C., Tsekouras, D., Antonakis, P., Sfiniadakis, J., Genetzakis, M., & Zografos, G. (2005). Gardner’s syndrome: A case report and review of the literature. World Journal of Gastroenterology, 11(34), 5408–5411. http://doi.org/10.3748/wjg.v11.i34.5408.
- Aletaha, M., & Fateh-Moghadam, H. (2012). Gardner Syndrome. Journal of Ophthalmic & Vision Research, 7(3), 257–260.
Further Reading
Last Updated: Mar 17, 2021