Parkinson’s disease (PD) is treated by levodopa, which is a prodrug capable of crossing the blood-brain barrier before being metabolized to dopamine, a vital neurotransmitter in the brain.
However, certain gut bacteria interfere with this treatment, leading to unpredictable fluctuations in the motor response to levodopa and pushing up the dosage levels unnecessarily.
Image Credit: CI Photos/Shutterstock.com
The Gut-Brain Axis
The gut microbiome numbers trillions, which is an order of magnitude higher than the number of cells in the human body. It also contains 150 times more genes and its biomass is equivalent to the human brain in mass. They are grouped into 500-1000 species belonging to 3 enterotypes, namely Ruminococcus, Bacteroides, and Prevotella.
All humans do not have the same microflora; in fact, not even all human populations do not share the same pattern. Variations occur in tune with the environment, nutritional factors, and genetic factors.
The mode of birth is thought to exert a formative effect on gut microbiota, in common with the maternal diet, neonatal health, maternal age, antibiotic exposure, and other factors that form antibiotic resistance determinants.
The gut microbiome functions to inhibit the growth of pathogenic bacteria, protect the gut epithelium from invasive growth, synthesize vitamins, modulate the energy balance of the body, regulate immune development, and xenobiotic effects.
They also produce essential molecules like short-chain fatty acids (SCFAs), bile acids, choline, amino acids, and other precursor molecules that maintain the integrity of the neurohormonal axis.
The gut-brain axis could be defined as a relationship between neurons in the gut, the peripheral nervous system, and the central nervous system.
Is PD Related to the Gut Microbiome?
Parkinson’s disease is a progressive neurodegenerative disorder in which there is a deficiency of dopamine in the substantia nigra due to the loss of dopaminergic neurons, and cholinergic neurons from the posterior motor nucleus of the vagus. Simultaneously, the brain shows an accumulation of alpha-synuclein.
PD is the second most common neurodegenerative condition in the world, affecting 1% of the world’s population in the over-60-year age group.
The gut neurons and gut microflora are related via several protein receptors that activate the innate immune system like the toll-like receptors (TLRs). In mice models, these are activated by the dysregulated hypothalamopituitary axis (HPA) occurring as a result of chronic stress.
The final event is dysbiosis of the gut, with a marked reduction in ‘good’ species like those of the genus Bifidobacterium, and the overgrowth of pathogenic species.
If this is prolonged, ‘leaky gut syndrome’ occurs, with increased intestinal permeability and colitis. Low-grade inflammation sets in, with the breakdown of the intestinal epithelium, and oxidative stress.
Immune reactions are suppressed, disrupting the blood-brain barrier, which in turn allows lipopolysaccharides from Gram-negative bacteria and other toxins to gain access to the brain. One of the resulting conditions is PD.
Do Gut Microbes Disrupt PD Treatment?
However, gut microbiota can also stop one of the drugs that are effective in the treatment of PD by breaking it down. Levodopa is a prodrug that is metabolized to dopamine in the brain.
However, gut microbes like Enterococcus faecalis break down much of the levodopa into dopamine before it ever crosses the epithelial barrier of the intestine. Unfortunately, dopamine cannot cross the blood-brain barrier.
Research has shown that a molecule similar to amino acid can block E. fecalis without killing it. The administration of this molecule results in increased levodopa levels, in mice.
This conversion of levodopa to dopamine is catalyzed by the enzyme tyrosine decarboxylase that is also responsible for converting tyrosine to tyramine. The rate of levodopa metabolism remains high even when this bacterium is exposed to a high concentration of tyrosine, which is an alternative substrate.
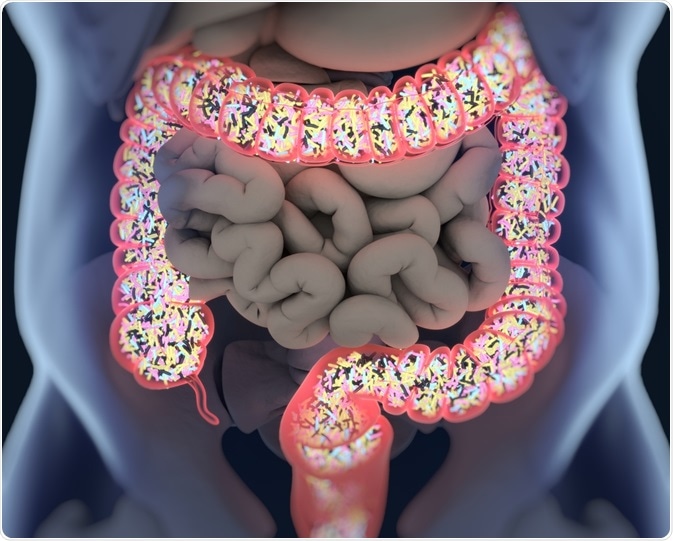
Image Credit: Anatomy Insider/Shutterstock.com
Decarboxylase Inhibitors Ineffective
Patients with PD receive a decarboxylase inhibitor like carbidopa to block this type of peripheral conversion of levodopa to dopamine. However, this only blocks the human version of this enzyme, leaving the bacteria unaffected.
Other compounds like benserazide and methyldopa are also ineffective at inhibiting the bacterial enzyme.
The resulting lower levels of levodopa reaching the brain may be one reason why levodopa is not uniformly effective in all patients. Fecal samples showing a high concentration of the bacterial tyrosine decarboxylase gene are found in patients who need higher doses of levodopa and carbidopa, as well as a longer period of treatment.
The Vicious Cycle: High Decarboxylase-High Dopamine-Bacterial Overgrowth
Many PD patients have slow intestinal motility, probably because of the higher levels of dopamine produced from levodopa. It could also be because of the overgrowth of small intestinal bacteria. It is linked with a variable motor response to the drug levodopa, which results in a higher frequency of dosage.
Again, the use of proton pump inhibitors to treat gut symptoms could lead to the overgrowth of levodopa-metabolizing bacteria.
The final common pathway for all these stimuli is bacterial overgrowth in the small intestine, triggering a vicious cycle. Moreover, long-term exposure to this combination of drugs may probably select for bacteria that express the genes encoding tyrosine decarboxylase, leading to its overgrowth.
Higher doses of levodopa can cause dyskinesia, a serious obstacle to achieving adequate dosages, and symptom control. Hope may come through the small molecule alpha-fluoromethyltyrosine (AFMT), that can block this pathway.
Says researcher Emily Balskus of Harvard University, “This opens up the door to the possibility of developing a new class of therapeutics to improve patient response to levodopa – that would be drugs targeting gut microbe metabolism in addition to targeting host metabolism.”
Sources
- Ilie, O.-D. et al. (2019). Minireview on the Relations between Gut Microflora and Parkinson’s Disease: Further Biochemical (Oxidative Stress), Inflammatory, and Neurological Particularities. Oxidative Medicine and Cellular Longevity Volume 2020. https://doi.org/10.1155/2020/4518023.
- Van Kessel, S. P. et al. (2019). Gut bacterial tyrosine decarboxylases restrict levels of levodopa in the treatment of Parkinson’s disease. Nature Communications 10, 310. https://doi.org/10.1038/s41467-019-08294-y
- Vaughan, A. (2019). Gut microbes interfere with Parkinson's drug - but we could stop them. Available at: www.newscientist.com/.../2206501-gut-microbes-interfere-with-parkinsons-drug-but-we-could-stop-them. Accessed on May 2, 2020.
- Rekdal, V. M. (2019). Discovery and inhibition of an interspecies gut bacterial pathway for Levodopa metabolism. Science, Vol. 364, Issue 6445, eaau6323.
DOI: 10.1126/science.aau6323
Last Updated: May 22, 2020