Harlequin ichthyosis (HI) is a rare, congenital skin condition. HI affects the skin over almost the whole body of an infant, and carries a high risk of neonatal death due to severe and life-threatening infection.
The incidence of HI is about one in every 500,000 people. Both males and females are affected equally.
Teenager Suffering From Rare Harlequin Syndrome
Genetics of HI
HI is caused by a mutation of the ABCA12 gene. This gene helps to direct the production of the ABCA12 protein involved in transporting fats within the epidermis, which is essential for normal skin synthesis. Various mutations in ABCA12 can occur, some of which can shut down the manufacturing of this protein, whereas others can induce the production of an abnormal form of the protein.
HI is inherited in an autosomal recessive fashion, which means that individuals with HI have two copies of the mutated genes; one inherited from each parent. If two people with the mutation have a child, there is a 25% chance that the child will be affected. Parents of children with HI are carriers of the mutated gene and show no sign of the disease, as they have one normal copy which compensates for the defective one.
Signs and symptoms
The skin is the largest organ of the body. Normal skin acts as a waterproof and protective, but highly flexible barrier between the body and the environment. The skin helps to regulate many of the body's functions and is responsible for the sense of touch. Taken together, the normal properties of the skin are challenged in HI.
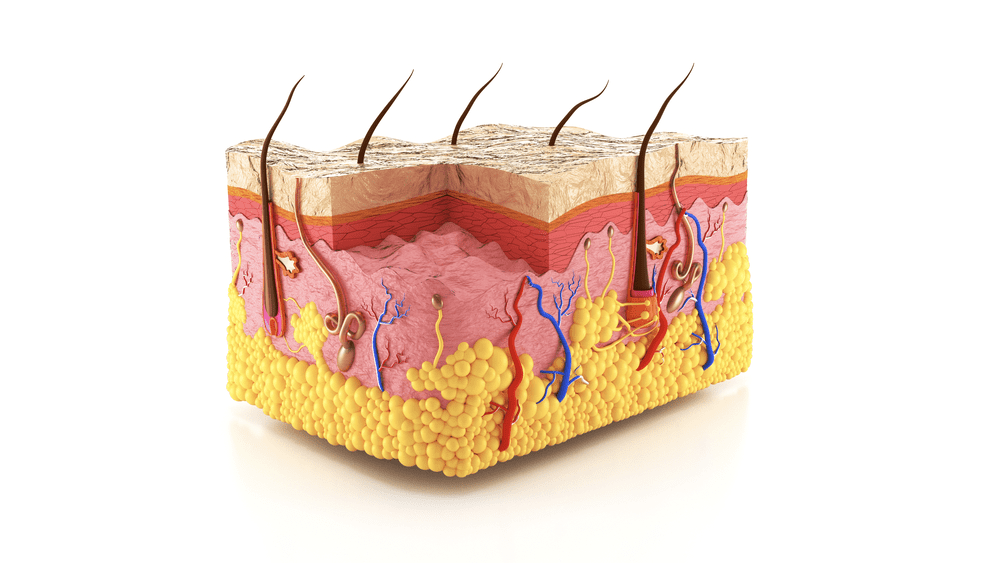
Image Credit: Anton Nalivayko / Shutterstock.com
In HI, premature birth is common. The infant is born encased in extremely thick skin that forms into large plates rather like armor, instead of a continuous sheet of thin and pliable skin. This appearance is due to the presence of an abnormally hard thickened integument, which is severely cracked or fissured. The cracks are so deep that it can even expose subcutaneous tissues.
An infant with HI faces life-threatening risks associated with preterm birth, as well as those due to the presence of numerous and deep skin fissures that result in the loss of the regulatory and protective functions of the skin.
For these reasons, the infant is usually placed in the neonatal intensive care unit (NICU) immediately after birth.
Complications of HI
External deformities
A child with HI typically exhibits an appearance that is distorted by the rigid skin. In fact, some infants may have no apparent external ears, or deformed ears, because the abnormal skin draws them tightly inwards.
The eyes and the eyelids are often affected in various ways. In some, the eyelids cannot close properly. In others the swollen eyelids obscure the eye area.
The mucous membranes of the eyes may be permanently exposed (ectropion) due to such anomalies, leading to the development of dry eyes.
Some neonates may have the eclabium, which is the red oral mucosa of the eye, exposed because the taut skin draws the lips outwards in a fixed grimace.
The hands and feet may be smaller than usual, with restricted mobility of fingers and toes.
Breathing
Individuals with HI often suffer from respiratory problems or even respiratory failure. This is due to the restriction of chest movement by the tight thick skin.
Eating
Infants born with this condition may have to be fed with a tube through the nose in early neonatal life, as their ability to suck and swallow is restricted.
Dehydration
The deeply fissured skin causes the loss of excessive amounts of salt and water, which may result in severe dehydration. This in turn affects the regulation of body temperature and may induce hypothermia.
Infection
Life-threatening infections may set in within the early days of life due to the entry of pathogens through the disrupted skin barrier.
Diagnosis and treatment
HI is diagnosed by the characteristic skin findings at birth or in infancy. In milder cases, it may resemble other diseases such as eczema.
HI can sometimes be diagnosed in utero by a 3D-ultrasonography. Neonates require a moist environment with careful handling in an isolated incubator at birth.
The skin should be kept soft by constant application of petrolatum-based creams. Older children should be treated with long daily baths with bath oils added to the water.
Lubricant ointments are required. Keratolytics are also used to peel off and reduce the thickness of the skin due to the excessive growth of the superficial stratum corneum. This will increase the softness and suppleness of the skin. Oral retinoids are useful in severe cases; however, their use should be monitored.
The thick plates of skin gradually peel off over several weeks. The skin appears very red and shiny from the peeling.
Physiotherapy benefits some patients who suffer from restricted mobility. Other treatments may be needed; for instance, counseling can help patients cope with the psychological challenges of the disease.
Other important aspects of HI treatment include the prevention of infection, dehydration and drying out of the cornea. When required, the skin may have to be incised to allow proper circulation and thoracic movement.
References
Further Reading
Last Updated: Aug 17, 2023