Hepatitis C virus (HCV) is an RNA virus that belongs to the Flaviviridae family. It was first detected in 1989 and is an enveloped virus that has a very limited range of hosts that includes humans and chimpanzees.
 Image Credit: Tatiana Shepeleva/Shutterstock.com
Image Credit: Tatiana Shepeleva/Shutterstock.com
Hepatitis C is a blood-borne infection and there are several genotypes of this virus that can infect humans leading to damage to the liver either in the short term or in the long term. These genotypes of the virus are defined according to the differences in the molecular structures of these viruses.
The incubation period of acute hepatitis C is usually between 6 and 9 weeks this means that it takes around 6 to 9 weeks for the infection to become evident after a person has contracted the virus. The routes of transmission of this infection are usually via blood and other body fluids.
Acute hepatitis C is usually asymptomatic and there may be no evidence of the illness. Transmission from these asymptomatic individuals who show no symptoms or signs of the infection is one of the reasons why this infection poses such a public health threat.
What is Hepatitis C and Why Should You Care?
Routes of transmission of hepatitis C virus
This infection is highly contagious. The smallest amounts of blood from an infected person, even if it has dried for up to two weeks can carry the infection. Hepatitis C virus can be transmitted from one infected person to another via these routes –
- Via blood transfusion. Blood from a person who has HCV infection carries the virus that can infect a recipient of the donated blood. Since September 1991 all the blood donated and received in UK has been screened for HCV. Blood transfusions prior to that may carry a risk of having transmitted HCV infection from an infected donor.
- Intravenous drug use using shared needles or hypodermic syringes carry a risk of transmitting the infection. Intravenous drug abusers commonly share needles and since many of these street drug users are essentially undetected cases of HCV infection, the risks of transmission are high.
- Patients undergoing hemodialysis for failing kidneys are put on machines that help purify their blood. The circuitry of these machines when used by an infected person carry the risk of transmitting it to non-infected persons.
- Needlestick injuries are common among healthcare workers. Just like HIV infection, HCV infection can also spread when a healthcare worker accidentally pricks himself or herself with a needle that has been used by an infected person. These injuries lead to an estimated 3% risk of HCV transmission.
- Transmission rates of HCV infection are significant from an infected mother to her baby during the process of birth. This is called perinatal transmission. The risk of transmission is around 6 % and this rises significantly if the mother is also infected with HIV.
- The risk of transmission of HCV is possible but rare when a non-infected person comes in sexual contact with a person with HCV. Less than 1% per year of a relationship risk exists due to sexual transmission of HCV. The rates however rise significantly if the infected partner has a co-infection with HIV as well.
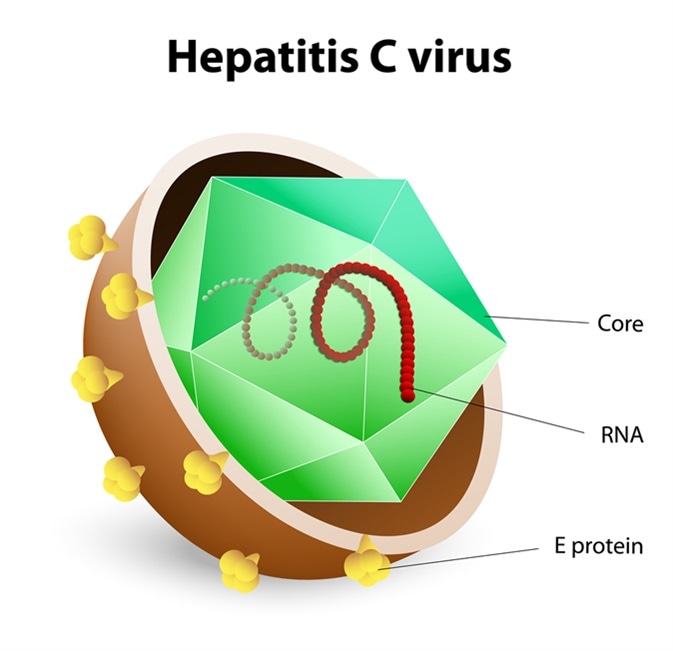 Image Credit: Designua / Shutterstock
Image Credit: Designua / Shutterstock
Due to the above-mentioned routes of transmission of hepatitis C, the risk factors associated with hepatitis C infection include;
- Injectable drug users remain the most important risk factor for getting HCV infection.
- Blood transfusions from HCV positive donors
- Pregnant mothers with the infection to their babies. Breast-feeding by infected is considered safe though.
- Sexual transmission of HCV is possible but cannot be ruled out. Persons with multiple sexual partners are at risk.
- Needlestick injuries among health care workers, social service workers, police, prison staff, etc.
- Those who undergo tattoos, piercings, acupuncture, etc. with unsterile needles are at risk of transmitting as well as getting HCV infection. Sharing toothbrushes with blood and razors with traces of infected blood can also raise the risk of infection.
References
Further Reading
Last Updated: Apr 13, 2021