As of January 5, 2020, approximately 1.86 million people have died from infection by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This unprecedented global health and economic crisis has led scientists to investigate alternative treatment approaches that might be able to treat and/or prevent the effects of this highly infectious disease, one of which includes monoclonal antibody therapies.
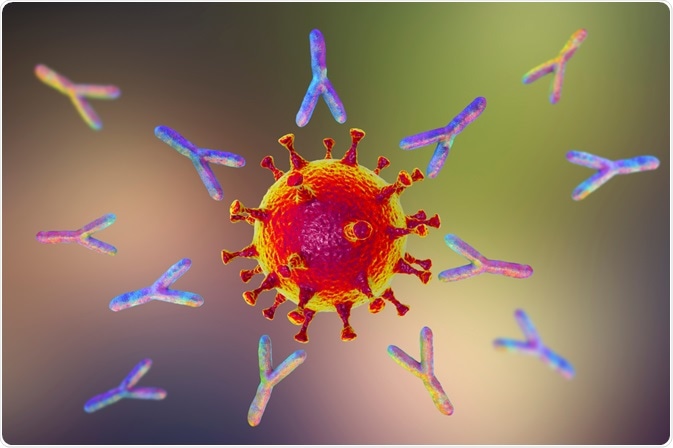 Image Credit: Kateryna Kon / Shutterstock.com
Image Credit: Kateryna Kon / Shutterstock.com
An overview of the SARS-CoV-2 structure
SARS-CoV-2 is a large enveloped RNA virus that contains a single-stranded and positive-sense RNA genome. The RNA genome of SARS-CoV-2 encodes for a number of different proteins that are both structural and non-structural in nature, in addition to several additional accessory genes.
The ability of the SARS-CoV-2 virus to fuse to mammalian cells is mediated by the envelope spike (S) protein, which is a trimeric type-1 integral membrane protein and class-1 fusion protein.
The S protein contains both S1 and S1 subunits, the first of which houses the receptor-binding domain (RBD), which binds to the angiotensin-converting enzyme 2 (ACE2) receptor present on cell membranes in order to mediate the entry of the virus into the host.
The interaction between the RBD and the ACE2 receptor results in the formation of the RBD-ACE2 complex, which subsequently causes the S protein to undergo a conformational change that ultimately leads to the fusion of the virus to the cell membrane.
Taken together, the S protein is of immunological interest, as researchers investigating potential treatments often look to target this aspect of the SARS-CoV-2 in order to prevent its infection and replication capabilities.
How do antibodies target SARS-CoV-2?
Once the SARS-CoV-2 virus has entered its host, the virus will replicate, which causes the adaptive immune system to initiate various cellular responses, which includes the generation of antibodies (Abs) such as neutralizing antibodies (NAbs), which are the primary type of Abs that are produced following infection by SARS-CoV-2.
These innate NAbs, which include IgM, IgG and IgA, are directed to the S proteins located on the surface of the virus molecule, as well as to the internal N proteins within a week following the onset of symptoms.
Can antibodies reduce the severity of SARS-CoV-2?
Unfortunately, conflicting results have been reported on the ability of Abs to reduce the severity of COVID-19. Although an inverse correlation has been reported between the viral loads and the production of SARS2 specific-Abs, several studies have found that by the time Abs develop, viral loads often decrease.
Additionally, those with smaller viral loads, which can often be present in those with mild or asymptomatic infections, often have a weak or totally absent Ab response. Furthermore, several studies have found a positive correlation to exist between specific-AB titers and the severity of COVID-19, thereby further supporting the notion that the Ab response is insufficient in preventing and/or reducing disease severity. Taken together, these two factors, therefore, point to the more significant role that innate and/or cellular adaptive immune responses have in partially controlling the virus.
On the other hand, several studies have oppositely confirmed the antiviral effect of certain Abs. These studies have found that seroconversion, which is defined as the first day in which a serological test turns positive for specific-Abs, occurs in most COVID-19 patients, and has reported occurring in up to 98.8% of patients in some studies.
Additional studies have also found that as anti-S immunoglobulin M (IgM) and IgG antibodies develop, the viral loads in SARS-CoV-2 infected patients are reduced. Clearly, there remains a lack of understanding surrounding the role that antibodies produced by the host might have in mitigating infection by SARS-CoV-2; therefore, the development of alternative therapeutic strategies that do not solely depend on the innate immune response is crucial.
 Image Credit: Lightspring / Shutterstock.com
Image Credit: Lightspring / Shutterstock.com
What SARS-CoV-2 antibodies have been used clinically?
In response to the SARS epidemic of 2003, several monoclonal Abs (MAbs) were developed; however, most of these Abs are not capable of neutralizing the SARS-CoV-2 virus, despite their similar structural characteristics.
Regardless of this setback, researchers from around the world have successfully developed several highly potent neutralizing MAbs that are capable of targeting the RBD and S protein of the SARS-CoV-2 virus. To date, four major SARS-CoV-2 MAbs have been isolated from COVID-19 convalescent patients, each of which targets the RBS and competes directly with ACE2 receptor binding.
These neutralizing MAbs have not only been investigated for post-exposure treatment, but also as a prophylactic measure. To date, a few SARS-CoV-2-targeting nAbs, which include both MAbs and polyclonal IgG, have progressed to clinical trials, which include SAB-185, VIR-7831, LY-CoV555, and a combination of REGN10933 and REGN10987. During the phase 2 trials on LY-CoV555, for example, a single infusion of 2800 mg of this antibody was found to effectively clear the virus by day 11 following diagnosis with mild to moderate COVID-19.
When administered together, the combination treatment of REGN10933 and REGN10987 was found to reduce COVID-19 related hospitalizations or emergency room visits in patients who are at a high risk for progressing to severe COVID-19, which included those who are above the age of 65 years or had certain chronic medical conditions.
These positive clinical trial results have led the United States Food and Drug Administration (FDA) to authorize the emergency use of LY-CoV555 (Blamnivimab), REGN10933 (Casirivimab) and REGN10987 (Imdevimab) as of November 2020.
Limitations
The use of therapeutic nMAbs is associated with various limitations in the clinical settings, all of which should be carefully considered prior to authorizing the use of these therapies in treating COVID-19 patients. Currently, the only way to administer nMAbs is through intravenous (IV) injection, which can be impractical in certain clinical situations.
Furthermore, IV injection also increases the risk that the patient will experience immune reactions, such as anaphylaxis, serum sickness, or even generation of antibodies against the drug itself. As a result of this limitation, researchers have studied the practicality of administering nMAbs through subcutaneous injections that could even be administered by the patient themselves.
In addition to administration challenges, MAbs can also induce a number of unwanted side effects as a result of their specific targeting sites that can alter the normal activities of certain endogenous immune mediators.
Although the SARS-CoV-2 therapeutic MAbs have been specifically designed to attack the exogenous viral epitopes, its potential to induce adverse events in the host must still be considered. Another challenge associated with antibody therapies is the high cost associated with manufacturing these types of drugs on a large scale.
References
Further Reading
Last Updated: Jan 20, 2021