Introduction
Psychological effects of infertility
Psychological effects in men
Psychological effects in women
Medication side effects
Financial concerns
Uncertainty about treatment outcomes
Conclusion
References
Further reading
Introduction
For women, infertility refers to when a woman under the age of 35 has failed to conceive, despite having had regular, unprotected sexual intercourse for one year. For women aged 35 to 40 years and over 40 years, infertility is the inability to conceive after six and three months of unprotected intercourse, respectively. Even the inability to carry a pregnancy to full term or recurrent pregnancy loss is infertility.
 Image Credit: Chanintorn.v / Shuttterstock
Image Credit: Chanintorn.v / Shuttterstock
Infertility is a common problem. Around 5% of couples in developed countries experience primary infertility, which describes an inability to conceive in the first place, or secondary fertility, which refers to when a woman has given birth previously but is currently unable to conceive or carry a pregnancy to term.
In the U.S., around 6% of married women aged between 15 and 44 years fail to achieve pregnancy after one year and about 12% of that age group, regardless of marital status, has impaired fecundity – the ability to conceive or carry a pregnancy to term.
Both sexes share the cause of infertility equally; 30% is male-factor infertility, and 30% is female-factor infertility. The rest 40% of cases fall under the category of "unexplained" infertility, in which both partners have a fertility issue, but all tests fail to identify a cause.
Various treatments are available to help infertile couples, ranging from medications that regulate ovulation to surgical procedures to treat endometriosis, for example, and assisted conception, which may be intrauterine insemination (IUI) or in vitro fertilization (IVF).
Psychological effects of infertility
Experts had previously thought that only around half of all problems with fertility were physical in origin, with the remainder being unexplained or a result of psychosomatic issues on the woman's part. However, research now shows that most infertility cases have a physical origin, which may involve one partner or both.
Although infertility is generally caused by physiology, possible psychological effects of infertility treatments can result in stress and heartache. For example, one study involving 200 couples visiting a fertility clinic showed that about 50% of the women and 15% of the men described infertility as the most distressing experience of their lives.
Psychological effects in men
Less research exists into the psychological impact on men, although studies to date have shown that men tend to report fewer feelings of distress than women. However, one study found that men's reactions to infertility may depend on which partner is diagnosed with a fertility problem. When the problem lies with the female, men do not report feeling the same degree of distress as women do, but men who find out they are themselves infertile report the same levels of depression and low self-esteem as females do.
In traditional cultures, fatherhood is regarded as the equivalent of manhood. Therefore, men often feel reluctant to talk to their male friends about their infertility diagnosis due to the association of infertility with virility and masculinity. The stigma surrounding infertile men often results in those with less education showing more substantial depressive symptoms. The diagnosis and infertility treatment requires frequent trips to clinics contributing to the medicalization of reproduction and the perception of being "sick" or "unhealthy" in otherwise healthy men. Men also find it tedious to undergo assisted reproductive treatments (ARTs), which require several blood tests, and semen analyses. Additionally, ARTs often require the man to produce a 'good' semen sample contributing to concerns about sexual functioning.
A recent study by Martins et al. (2016) quantitatively examined how men psychologically adjusted to infertility treatment. The study time frames varied from four weeks to five years post-treatment. They found that men reported increased depressive symptoms within a few weeks after the baseline assessment. In terms of coping strategies, it was found that active coping strategies decreased, and religiousness increased in men four months after the infertility work-up. Men also reported less social support and more negative reactions from family and friends one year after beginning the infertility treatment.
Luk and Loke (2015) also documented the occurrence of erectile dysfunction and diminished sexual interest following a diagnosis of male factor infertility. Also, studies found that psychological stress could reduce sperm density and progressive motility and increase the number of abnormal sperm.
While men process and cope with infertility diagnoses differently than women, their experiences deserve equal attention in the clinical and research realms.
Psychological effects in women
A study of 488 women, who completed questionnaires before taking part in a stress reduction initiative, concluded that infertile women experienced the same degree of depression and anxiety as people diagnosed with high blood pressure, cancer, or recovering from myocardial infarction.
Between 25% and 65% of women undergoing an ART have clinical symptoms of stress, anxiety, and negative emotions, such as low self-esteem or guilt. Stress that people suffer in their daily lives due to work or family reasons and the stress that is generated when feeling infertile and becoming an A.R. patient, all combined with the uncertainty of success or failure of the treatment, makes one "stagger."
A recent study showed that the patients receiving psychological support during the ART better handled the penalties and showed less treatment abandon (5.7%). They were livelier to try it more times and therefore had more probability of achieving their goal. They obtained 54% of pregnancies compared to the group that did not follow the program (28%).
Studies have shown that the physiological mechanisms related to stress and reproduction include centrally controlled gonadotropin-releasing hormone (GnRH) pulse inhibition as well as autonomic nervous system activation leading to alterations in ovarian and uterine function.
The sympathetic nervous system (SNS) and hypothalamic-pituitary-adrenocortical axis produce stress hormones. The SNS also stimulates the adrenal medulla to produce catecholamines (e.g., epinephrine). The short-term stress response can become an issue when it is experienced repeatedly or continuously. Chronic SNS stimulation also suppresses immunity by directly affecting cytokine profiles. In addition, during the stress effect, glucocorticoids (cortisol) are also formed from progesterone, which could alter progesterone, estrogen, and androgens production. Likewise, stress response compromises key functions in embryo implantation.
The complex relationship between psychological factors and fertility stress in women has become more and more recognized in the scientific literature as a factor that can negatively influence their reproductive capacity. In fact, it can become a determining factor in the case of at least 5% of infertility problems of unknown origin.
Lynch et al., pioneered the observation of an association of stress with reproduction. However, they could not establish the directionality of that association. Likewise, Louis et al. found that stress significantly reduced the probability of conception each day during the fertile window, possibly exerting its effect through the sympathetic medullar pathway.
The systems medicine, called predictive, personalized, preventive, and participatory (P4) model, has thus incorporated a P5, the "psycho-cognitive" aspects, to transform the ART recipient patients into active decision-makers. The fifth P analyzes the behavioral component, which helps patients decide between different therapeutic options and interact with clinicians in the treatment process.
Medication side effects
The medications used to treat infertility can cause a range of psychological side effects. The estrogen drug clomiphene, commonly prescribed to boost ovulation, can cause disrupted sleep, anxiety, irritability, and mood swings. Some other drugs can lead to mania, depression, and disrupted thought processes.
Hormone therapy effects include sleep disturbances, disruptions in sex drive, hot flashes, depressed mood, or anxiety, among other symptoms.
Both clinicians and patients may find it difficult to pinpoint whether the side effects are psychological or caused by medications, but it is essential to identify the cause in order to determine how to proceed.
Financial concerns
Infertility treatments can be extremely costly. In the U.S, the average cost is around $12,400 for a cycle of IVF, and this does not include medication or necessary 'add-ons.' Among individuals who cannot afford these costs or are not covered by insurance, not having access to treatment can contribute to feelings of hopelessness and helplessness. Even people with insurance may find the coverage is limited and must pay significant amounts. In addition, frequent medical appointments can cause worry about maintaining employment.
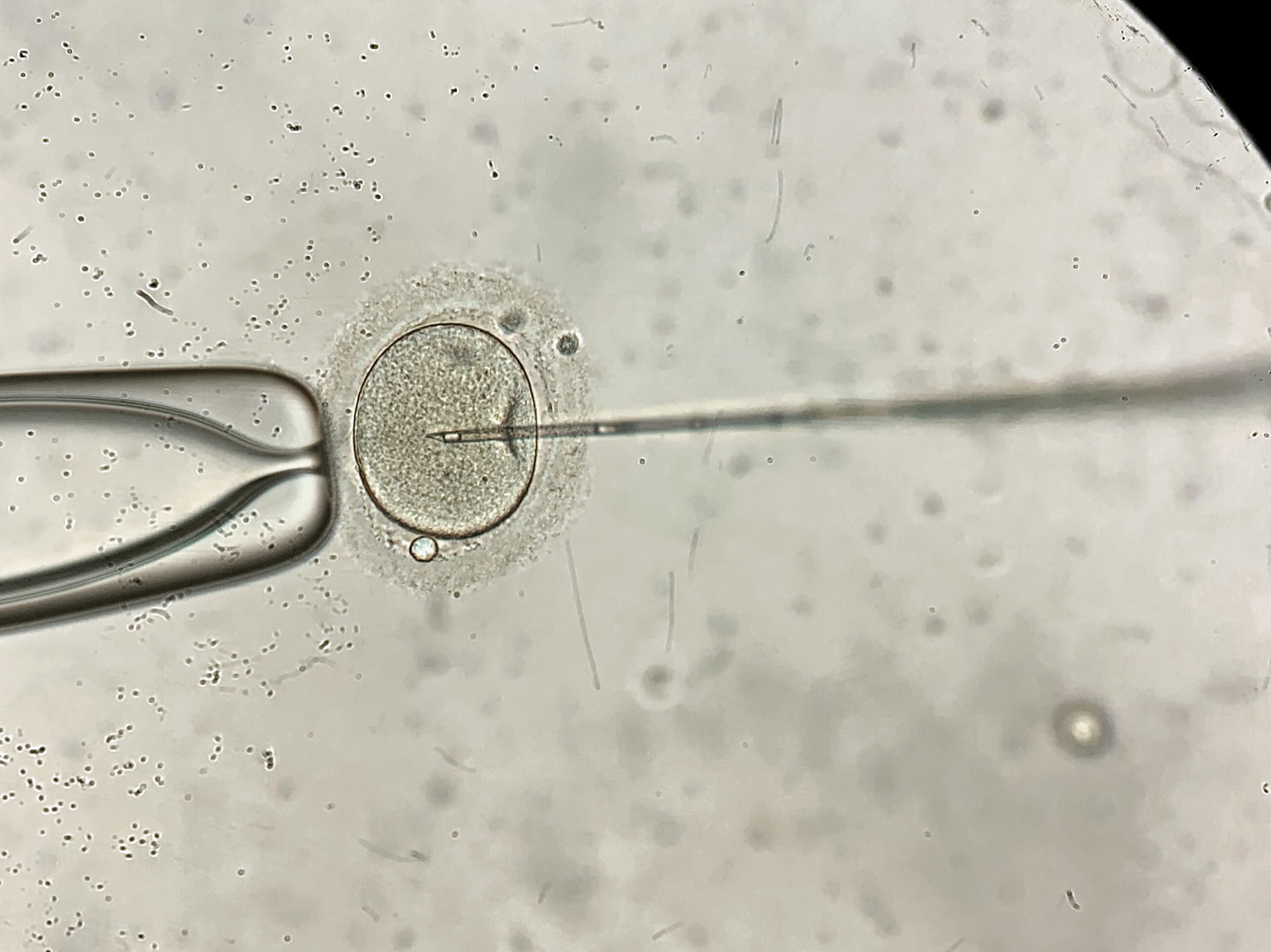 Process of the in vitro fertilization of a female egg inside IVF dish in the laboratory.. Image Credit: bezikus / Shutterstock
Process of the in vitro fertilization of a female egg inside IVF dish in the laboratory.. Image Credit: bezikus / Shutterstock
Uncertainty about treatment outcomes
Treatment interventions are effective in about half of the cases, although the likelihood of success decreases with increasing age. However, couples may lose emotional connection as fertility treatments continue. Fertility treatments also make sex less spontaneous, as it becomes focused on procreation rather than recreation.
If treatment fails, a couple may be overwhelmed with distress and grief, especially among individuals in Western countries, where the cultural assumption tends to be that hard work and persistence always lead to achievement and success. It can also be difficult for couples to know when they should stop treatment. Often, one partner will want to cease treatment before the other partner does, which can put a strain on the relationship. Many patients eventually have to come to terms with making a transition from wanting biological children to accepting that this is no longer possible.
Conclusion
To summarize, the psychological status of infertility patients should be assessed through structured interviews with a mental health professional or a valid questionnaire. It is also essential to provide patients with information and instruction on self-care skills that help them manage fatigue, resolve communication difficulties, and relieve anxiety. The first-line intervention could also include relaxation techniques, stress management, coping skills training, and group support. In cases where psychological treatment has not been effective for a patient and the symptoms of anxiety and/or depression are significant, a referral for a psychopharmacological evaluation is a must.
What is the Psychological Impact of Infertility? | Mira Lal
References
Further Reading
Last Updated: Apr 6, 2023