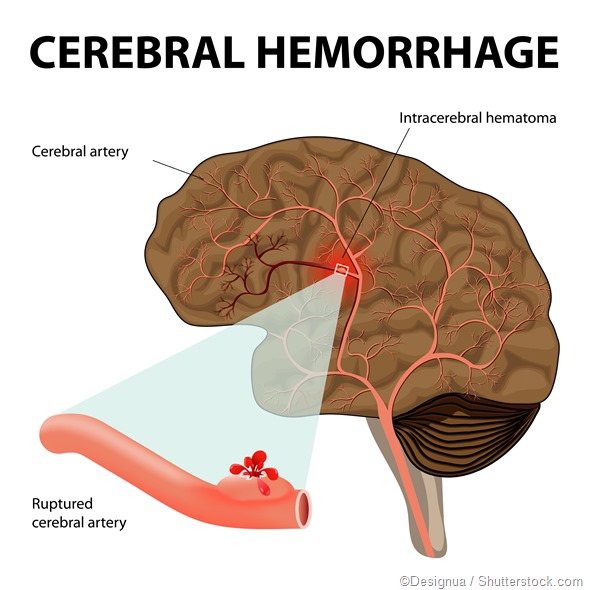
Intracerebral hemorrhage (ICH) is sudden, catastrophic bleeding that occurs in the brain tissue or ventricles. It usually results from damage to blood vessels due to hypertension. Symptoms are often sudden and severe. Loss of consciousness, vomiting, and headache are all common, but milder presentations are also possible, resembling ischemic stroke.
Causes of ICH include:
- Rupture of an aneurysm - when a blood vessel balloons out and bursts
- Cerebral amyloid angiopathy - accumulation of amyloid protein in the artery walls
- Thrombolysis
- Anticoagulant therapy
- Bleeding diathesis
- Hemorrhagic necrosis
- Cerebral venous thrombosis - when a blood clot blocks an artery in the brain, resulting in leakage from the damaged artery
- Trauma - car accident, fall, sports injury, etc.
- Bleeding tumor
- Conditions related to pregnancy like eclampsia, postpartum vas culopathy, neonatal intraventricular hemorrhage
Vascular lesions of the brain
A less common cause of ICH is a vascular lesion of the brain, such as an arteriovenous malformation (AVM) or aneurysm. An AVM is a tangle of dilated blood vessels that flow directly into veins. This often happens where cerebral arteries come together, but can also occur within the dura. AVMs may bleed or put pressure on brain tissue. If they are detected by neuroimaging, they might be correctable by microsurgery, radiosurgery, or endovascular surgery.
An aneurysm is a dilation of the artery which inflicts approximately 5% of people. A number of health conditions can increase the risk of aneurysm. Many brain aneurysms occur along the middle or anterior cerebral arteries. They also commonly appear in branches that communicate with the circle of Willis. Larger aneurysms may require treatment by endovascular therapy, if possible.
Epidemiology
ICH causes 8-13% of all strokes. Roughly 20,000 people die of ICH each year in the U.S.
Patients with ICH face greater mortality and likelihood of major disability than those with ischemic stroke or subarachnoid hemorrhage because the accompanying swelling can compress adjacent brain tissue. Its mortality rate after 30 days is 44%. If the hemorrhage occurs in the pontine or other brainstem area, that number climbs to 75% at 24 hours. African American people have higher incidences of ICH in the U.S. Higher rates have been found in China, Japan, and other Asian countries, potentially due to diet, environment, or genetics. Slightly more men than women suffer from ICH.
Rates of ICH increase in people older than 55 years, and double each decade until the age of 80 years.
ICH most commonly occurs in the lobar regions, thalamus, basal ganglia, cerebellum, pons, and other sites in the brainstem. Bleeding in the thalamic ganglion can extend into the ventricles. One third of ICH affect the ventricles of the brain.
Risk factors
Cigarette smoking, obesity, and diets high in fat and calories are all risk factors for ICH. Recreational use of cocaine and certain other drugs are also risk factors for ICH.
Diagnosis and treatment
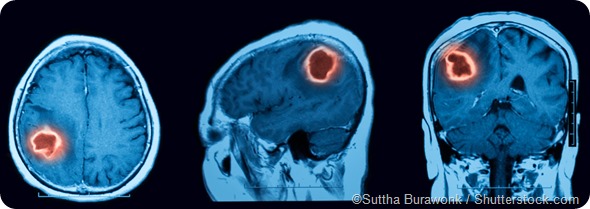
When symptoms of ICH are observed, neuroimaging should be carried out as quickly as possible - usually CT or MRI are performed. A lumbar puncture or CT angiography may also be necessary to confirm the diagnosis. Treatments include supportive care, reversal of anticoagulation therapy and surgical evacuation.
Sources
- Medscape, Intracranial Hemorrhage, http://emedicine.medscape.com/article/1163977-overview#a4
- Cleveland Clinic, Intracranial Hemorrhage, Cerebral Hemorrhage and Hemorrhagic Stroke, http://my.clevelandclinic.org/health/articles/intracranial-hemorrhage
- Merck Manual, Professional Version, Intracerebral Hemorrhage, https://www.merckmanuals.com/professional
Further Reading
Last Updated: Dec 29, 2022