Ketosis is a metabolic process that provides an alternative fuel source for the cells in the body during a low intake of carbohydrates. The hormonal changes associated with a low carbohydrate diet involve the reduction in the circulating levels of insulin, together with an increase in glucagon levels. These adaptations form a cornerstone of the ketogenic diet, which has gained a lot of popularity over recent years.
Ketogenic diet as treatment for epilepsy
Ketogenic diets are characterized by a reduction in carbohydrates (usually to the amount less than 50 grams per day) and a relative increase in the proportions of protein and fat. The pioneering work of Cahill and colleagues in the 1960s demonstrated the exact metabolic effects in classic ketogenic diets; however, this approach was already successfully used in the treatment of epilepsy in the early 1920s.
Principles of the ketogenic diet
Low-carbohydrate diets are considered to contain less than 100 grams or less than 30% of energy from carbohydrates per day. Such diets usually contain an increased proportion of the other macronutrients like proteins and fats; hence, the name “high-protein” or “high-fat” diets. Dietary fat can serve as caloric ballast and add to the taste.
The macronutrient composition of the diet is an important determinant of ketosis. The restriction of carbohydrates represents a more significant element of ketosis than the restriction of total calories. Ketosis is thought to occur when fat intake in the ketogenic diet exceeds twice the carbohydrate intake plus half of the protein intake.
Several mechanisms are proposed by which ketogenic low-carbohydrate diets may influence weight loss. Some of the initial weight loss is a result of diuresis, which encompasses both glycogen depletion and ketonuria; in turn, renal sodium and water loss are increased. Although it has been often stated that ketogenic diets suppress hunger, more research is needed to confirm this observation.
Ketone bodies also suppress appetite and create a metabolic advantage by increasing gluconeogenesis and up-regulating mitochondrial biogenesis. The latter denotes the formation of new mitochondria and subsequent production of extra energy. Other mechanisms include the limitation of food choices, the satiating effect of high-protein intake, increased adipose tissue lipolysis, increased fatty acid oxidation, and reduced palatability of low-carbohydrate diets.
As with any other fat-loss diet, exercise improves the success of the ketogenic diet. Still, high-intensity physical activity is unsustainable in a diet devoid of carbohydrates. Therefore, carbohydrates must be incorporated into the dietary regimen without disrupting the effects of ketosis. Modified approaches for such cases are known as the targeted ketogenic diet and the cyclical ketogenic diet.
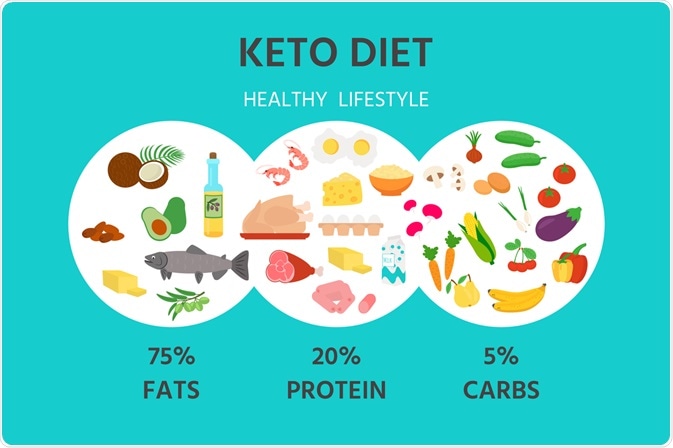
Image Credit: kos911 / Shutterstock.com
Therapeutic roles
A long-term ketogenic diet can significantly reduce body weight and body mass index without any significant side effects. In addition, it can also reverse the risk of heart disease, primarily due to the improvement of lipid profiles. More specifically, a long-term keto diet can lower blood pressure, low-density lipoprotein (LDL) cholesterol, which is colloquially known as the “bad” cholesterol, and increase high-density lipoprotein (HDL) cholesterol, which also known as the “good” cholesterol.
Since 1920, the ketogenic diet has been used as an effective approach in the treatment of severe childhood epilepsy; however, the interest in this treatment approach waned following the introduction of anticonvulsant drugs.
Today, the ketogenic diet can be considered as an option for children with intractable epilepsy who use multiple antiepileptic drugs. This diet is also a treatment of choice for seizures associated with glucose transporter type 1 deficiency syndrome (i.e. De Vivo disease).
Individuals with insulin resistance type 2 diabetes and metabolic syndrome are likely to see symptomatic and objective improvements in biomarkers of disease risk after introducing a well-formulated ketogenic diet. Glucose control improves not only as a result of less glucose coming in but also due to the increased sensitivity of cells to insulin.
The metabolic effects of a ketogenic diet lead to higher-than-usual oxidation of fats, which suggests reduced respiratory exchange ratio values. This can lead to potentially useful effects of this diet in patients with increased carbon dioxide as a consequence of respiratory failure. More research is needed to evaluate the effectiveness and safety of the ketogenic diet in other conditions.
References
Further Reading
Last Updated: May 21, 2021