Leukodystrophies are inherited disorders that are characterized by a progressive breakdown of the white matter in the central nervous system (CNS).
This breakdown of white matter, which is otherwise known as hypomyelination or demyelination, is due to several different mechanisms involving myelin proteins, as well as lipid and organic acid metabolism. They have to be distinguished from the “umbrella” term leukoencephalopathy, which is used to delineate any disease of the white matter.
Leukodystrophies are genetic in nature and, with a reported incidence of 1 in 7,500 live births, an ongoing public health issue in developed and developing nations alike. In younger individuals, these diseases are a significant cause of progressive neurologic disability; thus supporting the need for early and correct diagnosis of this condition.
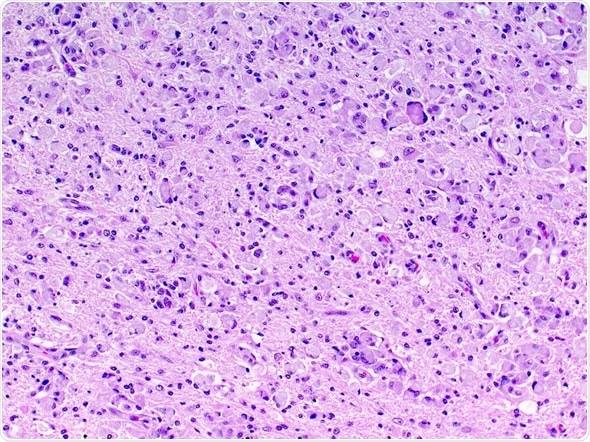
Image Credit: vetpathologist / Shutterstock
Pathophysiology and classification of leukodystrophies
A majority of leukodystrophies are monogenetic disorders, affecting the gene that usually encodes a protein or an enzyme that maintains neuronal health and is responsible for regulating brain metabolism. As many of these enzymes play a role in lipid metabolism, the ineptitude to synthesize or degrade a substrate leads to a downstream lack or an upstream excess of vital lipids.
This can in turn result in a wide array of pathologies, ranging from inflammatory demyelination to the degeneration of axons and activation of microglia. Therefore, the aforementioned demyelination or hypomyelination events are one type of manifestation that can be seen in leukodystrophies, as the myelinating oligodendrocytes are not the only cells affected in these conditions.
The major leukodystrophy disorders involve abnormal transport or degradation of myelin and oligodendrocyte sphingolipids, or of the myelin proteins. The abnormal processing of the metabolites can take place in the lysosome, at the peroxisome level, or can affect the adequate functioning of mitochondria.
Examples of lysosomal disorders include metachromatic leukodystrophy, globoid cell leukodystrophy or Krabbe disease, and various mucolipidoses and gangliosidoses. X-linked adrenoleukodystrophy is a peroxisomal disorder, while spongiform leukodystrophy, which is otherwise known as Canavan disease, as well as trichothiodystrophy, or Menkes syndrome, affect the mitochondria.
Clinical presentation
The dominant symptoms of leukodystrophy are neurological and, with several exceptions, appear in previously healthy children. Their onset is usually insidious in nature, with slow progression of symptoms and possible periods of stagnation. Unexplained and somewhat vague progressive mental and motor symptoms in a young person should raise suspicion towards leukodystrophic disorder.
A majority of patients with leukodystrophies do not present with any physical abnormalities. Dental abnormalities and large head, the latter of which is most notable in megalencephalic leukodystrophy and Canavan disease, can be observed. Comparatively, dysmorphic characteristics and skeletal abnormalities are rarely observed in metachromatic leukodystrophy with sulfatase deficiency.
As previously mentioned, progressive motor symptoms, particularly spasticity and cognitive changes, are the primary neurological symptoms of leukodystrophies. Very rarely, seizures can be observed as a late manifestation, and the involvement of peripheral nerves can lead to a combination of spasticity and diminished muscle stretch reflexes.
Diagnosing Leukodystrophies
After leukodystrophy has been considered as a possible diagnosis, establishing which kind of leukodystrophy is present usually entails obtaining an adequate medical and exhaustive family history, performing physical and neurologic examinations, reviewing magnetic resonance imaging (MRI) findings of the brain, but also pursuing specialized laboratory testing, such as molecular genetic testing.
MRI of the head represents the most important supporting test in a patient that is suspected of having a leukodystrophy. Minimal requirements for a standard interrogation are T1 and T2-weighted, as well as fluid-attenuated inversion-recovery (FLAIR) images.
However, since leukodystrophies habitually present before any obvious clinical and radiologic features are obvious, current strategies for diagnosis based exclusively on MRI criteria are deficient. Furthermore, MRI-based diagnostic approaches have not been evaluated for their sensitivity and specificity, and are highly dependent on skilled interpretation.
Care for Children with Leukodystrophies
Management and prognosis
Patients with leukodystrophies are gravely affected by the disease, with almost half requiring feeding tubes, and just over half are ever able to walk independently. Although primary treatment is usually not an option, the management of symptoms can ameliorate the comfort of individuals with these disorders.
In ideal situations, the patient with leukodystrophy is managed in a multidisciplinary way by experienced health providers. Intensive physical therapy improves function and mobility, with special attention given to the prevention and treatment of orthopedic problems.
Pharmacological agents can be used to adequately manage muscle tone and treat seizures that might be present. Augmentative communication is used to address speech deficits. Moreover, the emphasis should be on educational, nutritional, and recreational programs.
The prognosis ultimately depends on the specific type of leukodystrophy, albeit clinical cognizance of late-onset leukodystrophies should be strengthened, as new therapeutic modalities have been researched and developed. Some of the novel treatment approaches include gene therapy, enzyme replacement, and stem cell transplantation.
References
Further Reading
Last Updated: May 18, 2023