Light therapy has become one of the most exciting fields in biomedical sciences. Applications of intense pulsed light and lasers play an important role in clinical practice with a growing demand. During the last century, a plethora of light sources was introduced to treat or ameliorate acne symptoms.
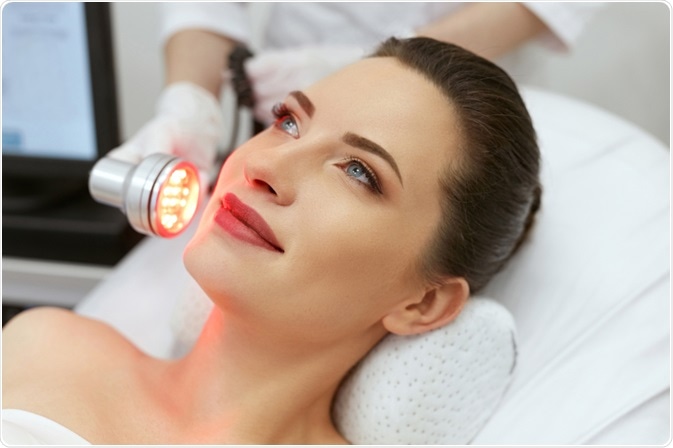
Image Credit: puhhha / Shutterstock.com
Acne vulgaris is one of the most common problems for which patients seek dermatologic care. It represents a disorder of the pilosebaceous follicles in the face and upper trunk. The disease burden of acne ranges from facial scarring to psychological, social, and emotional distress, with an almost inevitable self-perception of poor health.
Light and laser therapy
Light therapy of acne is based on the observation that the anaerobic bacterium Propionibacterium acnes is capable of synthesizing chromophores such as porphyrins, the main one of which is coproporphyrin III. Activation of porphyrin by a wavelength of 420 nanometers (nm) or less of light generates free radicals, which, in turn, leads to structural membrane damage and cell death.
Blue light can efficiently inactivate the aforementioned bacterium, but it is unable to penetrate the skin very far. Conversely, red light, which is less effective at exciting porphyrins, can reach deeper sebaceous glands and may exert an anti-inflammatory effect by inducing cytokine-release from macrophages. Thus, studies show the effectiveness of combined blue-red light therapy in reducing the number of inflammatory lesions.
Intense pulsed light (IPL) devices, which were introduced commercially in 1994, employ polychromatic light. IPL devices consist of flash lamps and computer-controlled capacitor banks, which generate pulsed polychromatic light. Its effects lead to photothermolysis, where endogenous chromophores in the skin create heat and energy from absorbing the light in order to target the blood vessels that supply sebaceous glands.
Lasers are also used in acne therapy. As compared to light therapy, lasers have the ability to concentrate coherent light on a smaller area of tissue. Potassium titanyl phosphate (KTP) 532 nm green light pulsed laser therapy is often used for that purpose, as it penetrates deeper than blue light and activates porphyrins to target Propionibacterium acnes.
Photodynamic therapy
Photodynamic therapy (PDT) embraces the use of three factors that include a photosensitizer, light, and oxygen. Aminolevulinic acid (ALA), methyl-aminolevulinic acid (MAL), indocyanine green (ICG), and other photosensitizing agents, such as indole-3-acetic acid, are used to enhance the effect of subsequent light or laser therapy.
Topical ALA enters epithelial cells where it is converted to protoporphyrin IX via heme synthesis pathway, accumulating both in the epithelium and pilosebaceous units. Illumination after ALA treatment leads to photoactivation of protoporphyrin IX and the production of singlet oxygen and cytotoxic free radicals.
This results both in the destruction of Propionibacterium acnes and the damage of the pilosebaceous unit. Important variables that influence the photoinactivation of this bacterium include the concentration of porphyrins, wavelength of discharged photons, temperature at which the reaction is carried out, and the availability of the tissue oxygen.
As an alternative to ALA, MAL is a lipophilic derivative of ALA that, in several studies, demonstrated superior penetration and selectivity in skin lesions. MAL has also been shown to be effective at reducing inflammatory lesions, but it can also, like ALA, lead to adverse effects including pain, skin swelling, erythema, and exfoliation.
References
Further Reading
Last Updated: Mar 11, 2023