Introduction
Epidemiological trends
Biological differences
Diagnostic challenges
Prevention and awareness
Future research directions
Conclusion
References
Further reading
Lung cancer has been widely perceived as a disease that predominantly affects men. However, recent epidemiological data indicate that it is increasingly being diagnosed in women. In fact, a large proportion of lung cancer cases are being diagnosed in non-smoking women, highlighting the importance of continued research in this area.
Introduction
Historically, men have been more likely to be diagnosed with lung cancer than women, but recent trends show a shift in this pattern.1-2 In 2019, men were still 23% more likely to be diagnosed with lung cancer compared to women; however, the incidence of lung cancer has been decreasing more rapidly in men than in women over the past decades.1-2
Young women are being diagnosed with lung cancer at higher rates than men in the same age group in several high-income countries.2 This shift has been associated with increases in adenocarcinoma cases in women, a type of lung cancer associated with smoking.3

Image Credit: PeopleImages.com - Yuri A/Shutterstock.com
Disparities in lung cancer incidence exist across different age groups, races, and histological types. For instance, women under the age of 54 have been observed to have higher incidence rates of lung cancer than men.4
Furthermore, it is notable that smoking behavior differs between genders, with men generally starting to smoke earlier in life. Despite this, women have been found to have higher odds ratios for major lung cancer types at every level of exposure to cigarette smoking. This practice appears to impact the risk of lung cancer in females more profoundly.5-6
Conversely, other factors must be involved in lung cancer development in non-smoking women.
Epidemiological trends
Lung cancer rates are now higher in women aged 35-54 than men of the same age in many high-income countries, despite declining smoking rates among both sexes.7-8
According to research, lung cancer diagnoses in women have increased by 84% in the last 43 years while decreasing by 36% in males, despite the fact that many of those women never smoked.7 In fact, women who have never smoked have more than twice the risk of developing lung cancer as males who have never smoked.7
A number of exogenous factors have been the subject of research into their potential influence on lung cancer development in non-smoking women.9 These include radon exposure in residential settings, secondhand smoke, high exposure to polycyclic aromatic hydrocarbons (PAHs) produced by cooking oils in poorly ventilated areas, and exposure to asbestos.9-10
Indeed, previous exposure to radiation for the treatment of other types of cancer, as well as infection with the human papillomavirus (HPV), has been associated with the development of this pathology.9
Lung Cancer in Women
Biological differences
In addition to exogenous factors, there are also endogenous factors that influence the development of lung cancer in women. These include specific genetic polymorphisms and estrogen exposures.
Research has indicated that women with lung cancer have impaired DNA repair mechanisms compared to men.3 This has been linked to polymorphisms in the cytochrome P450 gene (CYP1A1).3,9 Overexpression of the X-linked gastrin-releasing peptide receptor (GRPR), as well as mutations in the TP53 gene, have both been associated with an increased risk of lung cancer in women.3,9
Furthermore, women are at an elevated risk of developing lung cancer with a driver mutation, particularly in the EGFR, ALK, and KRAS genes.3,9 Nevertheless, the precise influence of a family history of lung cancer on its development in women remains to be elucidated.3,9
Conversely, women who are premenopausal and, therefore, produce higher levels of estrogen are more likely to be diagnosed with advanced lung cancer, specifically adenocarcinoma, than postmenopausal women.9 Furthermore, it is often observed that estrogen receptors are overexpressed in lung cancers.9
Nevertheless, the effect of estrogen in premenopausal women and hormone replacement therapy in postmenopausal women on lung cancer cells remains uncertain, with studies showing conflicting results.9
Stay Informed: Learn About the Lung Cancer Risk Factors
Diagnostic challenges
The current lung cancer screening guidelines, which are primarily based on smoking history, are inadequate in addressing the rising incidence of lung cancer in non-smoking women.10
The most recent guideline revisions have broadened the eligibility criteria for low-dose computed tomography (LDCT) screening, yet a substantial proportion of women remain ineligible for this form of screening.9-10 This has been partially justified by the potential harms of radiation exposure from LDCT, which necessitates the implementation of informed screening practices.9-10
Although the updated guidelines permit a broader diagnosis, future research should focus on incorporating diverse risk factors beyond smoking and investigating sex-specific differences in lung cancer, ultimately benefiting a larger population of women.9-10
Prevention and awareness
Lung cancer represents a significant concern for women, with an estimated 238,340 new cases expected in 2023.11 Alarmingly, 98% of women do not perceive it as a serious health risk despite early detection being crucial for survival.11
The Women and Lung Cancer Research and Preventive Services Act of 2023, supported by the ACS CAN, aims to address this through research, prevention, and awareness campaigns.11 These initiatives prioritize lung cancer in women through smoking cessation, addressing workplace risks, expanding screening access, and community engagement.11 An example of one of these initiatives is the "Plus One" campaign.11-12
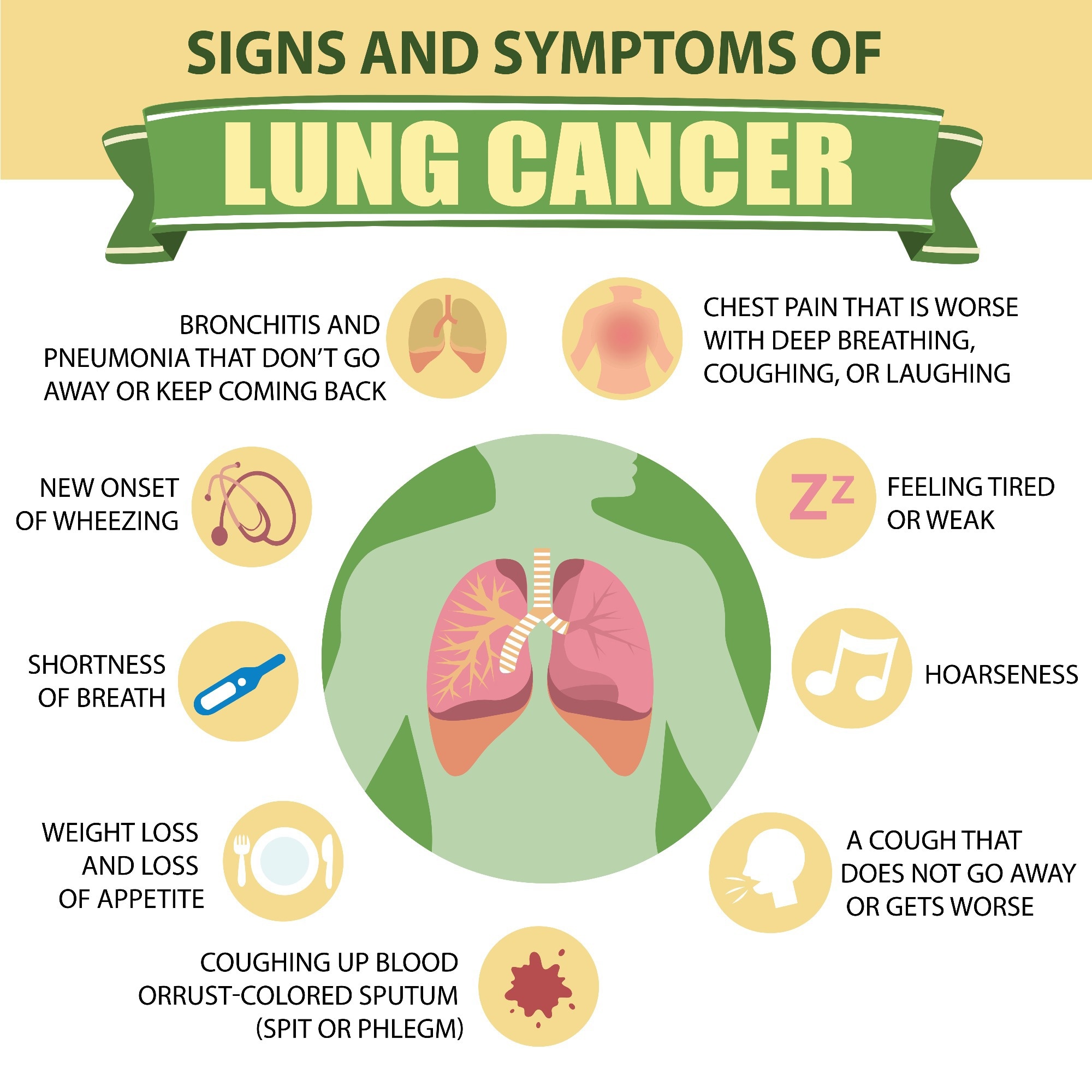
Learn about the signs and symptoms of lung cancer. Image Credit: Torrenta Y/Shutterstock.com
Future research directions
Lung cancer is the leading cause of cancer-related mortality among women globally. Yet, research remains limited.13 Key areas requiring further exploration include women-specific risk factors such as indoor pollution, secondhand smoke, biological differences, and treatment responses.13
The lack of female representation in clinical trials hinders the development of targeted therapies.13 Additionally, the surge in lung cancer among women, particularly non-smokers, remains poorly understood.13
Future research must prioritize understanding how sex differences impact lung cancer development and treatment response. This should include exploring avenues such as TLR2 activity and early-stage tumor biology, with the ultimate goal of improving outcomes for women.14
Conclusion
To address the disparities in lung cancer incidence and mortality among women, it is imperative to close the gaps in research and develop a more comprehensive understanding of the disease's unique impact on the female population.
This includes expanding clinical trials, exploring sex-specific biological mechanisms, and improving screening guidelines to reflect the rising incidence in women.
References
- Lung Cancer Trends Brief: Prevalence and Incidence. (n.d.). [Online]. Available at: https://rb.gy/y23ekp
- Dalmau, R. (n.d.). Women and tobacco, a gender perspective. [Online]. Available at: https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-20/women-and-tobacco-a-gender-perspective#:~:text=Tobacco%20consumption%20in%20women%20is,%25%20in%20low%2Dincome%20countries.
- Fidler‐Benaoudia M. M, et al. (2020). Lung cancer incidence in young women vs. young men: A systematic analysis in 40 countries. International Journal of Cancer, 147(3), pp.811–819. https://doi.org/10.1002/ijc.32809
- Fu Y, et al. (2023). Gender disparities in lung cancer incidence in the United States during 2001–2019. Scientific Reports, 13(1). https://doi.org/10.1038/s41598-023-39440-8
- Zang, E. A., and Wynder, E. L. (1996). Differences in Lung Cancer Risk Between Men and Women: Examination of the Evidence. JNCI Journal of the National Cancer Institute, 88(3–4), pp.183–192. https://doi.org/10.1093/jnci/88.3-4.183
- Gee, K., and Yendamuri, S. (2024). Lung cancer in females—sex-based differences from males in epidemiology, biology, and outcomes: a narrative review. Translational Lung Cancer Research, 13(1), pp.163–178. https://doi.org/10.21037/tlcr-23-744
- Christensen, J. (2023) Higher rates of lung cancer in women are a mystery for researchers, CNN. [Online]. Available at: https://edition.cnn.com/2023/10/13/health/lung-cancer-young-and-middle-age-women/index.html#:~:text=Smoking%20rates%20have%20declined%20significantly%20over%20the%20past%20couple%20of%20decades%2C%20according%20to%20the%20US%20Centers%20for%20Disease%20Control%20and%20Prevention%2C%20yet%20the%20cancer%20rate%20among%20women%20has%20inversely%20increased%20%E2%80%93%20particularly%20among%20women%20who%20have%20never%20smoked.
- Percentage of tobacco smokers worldwide from 2000 to 2025, by sex. (2024).[Online]. Statista. Available at: https://www.statista.com/statistics/937314/tobacco-smoking-prevalence-globally-by-gender/
- Ragavan, M., and Patel, M. I. (2022). The evolving landscape of sex-based differences in lung cancer: a distinct disease in women. European Respiratory Review, 31(163), 210100. https://doi.org/10.1183/16000617.0100-2021
- Lennon, A. (2022). Women and lung cancer: Should screening guidelines change? [Online]. Available at: https://www.medicalnewstoday.com/articles/women-and-lung-cancer-should-screening-guidelines-change#Risk-factors-beyond-smoking
- ACS CAN Supports the Women and Lung Cancer Research and Preventive. (2023). [Online]. American Cancer Society Cancer Action Network. Available at: https://www.fightcancer.org/policy-resources/acs-can-supports-women-and-lung-cancer-research-and-preventive-services-act-2023#:~:text=In%202023%20alone%2C%20an%20estimated%20238%2C340%20new%20cases%20of%20lung%20cancer%20will%20be%20diagnosed%20and%20an%20estimated%20127%2C070%20people%20will%20die%20from%20the%20disease
- Calgaro, A. (2024). LCRF, American Lung Cancer Screening Initiative join forces for "Plus One" campaign. [Online]. Lung Cancer Research Foundation. Available at: https://www.lungcancerresearchfoundation.org/lcrf-alsci/#:~:text=With%20the%20%E2%80%9CPlus%20One%E2%80%9D%20campaign%2C%20ALCSI%20will%20leverage%20its%20more%20than%2050%20chapters%20at%20universities%20across%20the%20United%20States%20to%20engage%20students%20in%20a%20grassroots%20effort%20to%20increase%20lung%20cancer%20screening%20awareness
- Florez N, et al. (2024). Lung Cancer in Women: The Past, Present, and Future. Clinical Lung Cancer, 25(1), pp.1–8. https://doi.org/10.1016/j.cllc.2023.10.007
- Millar F. R, et al. (2022). Toll-like receptor 2 orchestrates a tumor suppressor response in non-small cell lung cancer. Cell Reports, 41(6), pp.111596. https://doi.org/10.1016/j.celrep.2022.111596
Further Reading
Last Updated: Jun 3, 2024