Inflammation of the liver is known as hepatitis. Hepatitis can be of many types, including hepatitis A, hepatitis B, hepatitis C, and autoimmune hepatitis. Infection with the hepatitis B virus (HBV) is one of the most common health problems in the world.
In China, the prevalence of HBV infection among women of reproductive age may be as high as 2–8%, whereas it is only 0.4% in the United States. The majority of pregnant women who have HBV infection are chronic carriers, as evidenced by a positive hepatitis B surface antigen (HBsAg) status in their blood. The ovarian follicle and placental capillary endothelium have both been reported to express HBsAg.
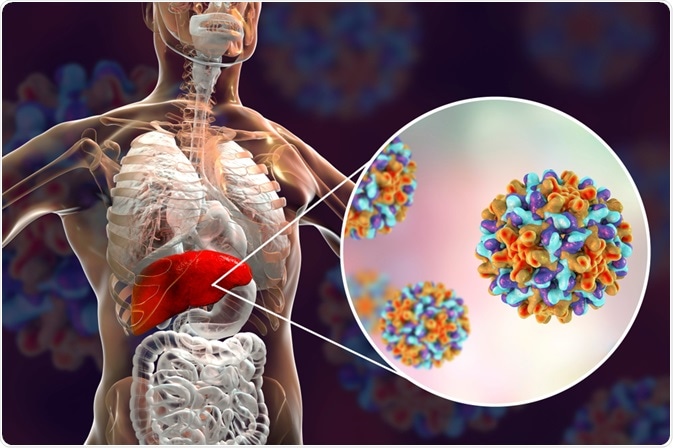
Image Credit: Kateryna Kon/Shutterstock.com
Significance of hepatitis in maternal health
Although all hepatitis viruses can harm the mother and child, acute hepatitis A virus or hepatitis E virus infection during pregnancy poses the greatest risk to maternal health and, as a result, to the fetus.
Hepatitis B virus (HBV), hepatitis C virus (HCV), and hepatitis D virus (HDV) major hazards, on the other hand, are linked to the severity of the mother's underlying liver disease and the risk of HBV and HCV mother-to-child transmission (MTCT).
To reduce the worldwide burden of chronic viral hepatitis, MTCT prevention is critical, and prevention programs must account for local healthcare and socioeconomic difficulties.
Pregnancy and hepatitis A
Hepatitis A is commonly seen in underdeveloped countries. Acute Hepatitis A virus infects 1 in 1000 pregnant women. With a mortality rate of 0.3 percent to 0.6 percent, the condition is largely self-limiting.
Premature contractions, placental separation, premature rupture of membranes, and vaginal bleeding have all been linked to hepatitis A during pregnancy. These findings were published in a study looking at the effects of acute hepatitis A on pregnancy.
Pregnancy and hepatitis B
Hepatitis B is a viral infection of the liver that can be acute or persistent. When people are initially infected with HBV, they usually don't have any symptoms. A percentage of people get chronic infections, which can advance to liver disease and lead to cirrhosis (liver scarring) or liver cancer.
A pregnant woman's hepatitis B virus (HBV) infection poses a substantial risk to her unborn child. The majority of infants infected from their mothers or before the age of five years develop chronic infection. Those who are infected after the age of five are far less likely to develop a persistent illness (only 5%).
In patients with acute or chronic HBV infection, the Hepatitis B virus has a rare negative effect on pregnancy. Hepatitis B virus infection during pregnancy is linked to an increased risk of maternal and perinatal death. Chronic HBV during pregnancy has been linked to placental abruption, premature birth, gestational hypertension, and fetal growth restriction.
Cirrhosis is more likely to develop in women who have chronic HBV during pregnancy. Without postexposure immunoprophylaxis, around 40% of infants delivered to HBV-infected mothers in the United States will develop chronic HBV infection, with one-fourth of those developing chronic liver disease.
In the absence of preventive measures, the probability of transmission from mother to child varies from 70% to 90% for women with a high HBV viral load (or who are HBeAg-positive), and from 10% to 40% for moms who are HBeAg negative. Even among newborns who receive the hepatitis B vaccine, high maternal quantities of HBV DNA (viral load) are linked to an increased risk of transmission.
As a result, pregnant women with high HBV DNA levels may benefit from antiviral prophylaxis throughout pregnancy to prevent mother-to-child transmission and avoid infection in their infants. Identifying HBV-infected (i.e., hepatitis B surface antigen [HBsAg]-positive) pregnant mothers and delivering hepatitis B immune globulin and hepatitis B vaccine to their infants within 12 hours of birth can help reduce perinatal HBV transmission.
Hepatitis C in pregnancy
More than 170 million people across the globe are infected with the hepatitis C virus. HCV infection affects about 8% of pregnant women. In HCV-infected pregnant women, gestational problems include fetal growth restriction, brachial plexus injury, fetal discomfort, cephalohematoma, neonatal convulsions, and intraventricular hemorrhage.
Hepatitis C virus (HCV) transfer from mother to child is rather rare. Antibody to HCV (anti-HCV) is found in 0.1 percent to 2.4 percent of pregnant women, while it is significantly higher in some endemic areas. The percentage of women with anti-HCV who have active viremia infection varies between 60% and 70%.
Only when serum HCV RNA is detectable, which may be linked to higher virus levels, the HCV transmission begin (above 106 copies per mL). In women with HCV viremia, the rate of mother-to-infant transmission ranges from 4% to 7% every pregnancy. Co-infection with the human immunodeficiency virus (HIV) boosts transmission rates by 4 to 5 times. The exact timing of transmission and mode of transmission are unknown.
Autoimmune hepatitis in pregnancy
The maternal and fetal outcomes of pregnant autoimmune hepatitis (AIH) patients are mainly unknown. The goal of a recent meta-analysis was to identify the level of evidence linked with maternal and fetal outcomes in AIH patients. They performed a comprehensive search of the literature.
Patients with AIH who had at least one pregnancy with a previously known or index presentation diagnosis of AIH were included in the trials. The researchers utilized a random-effects model with 95% confidence intervals (CI) and odds ratios (OR).
The treatment of viral hepatitis in the context of pregnancy necessitates extra caution. Hepatitis A, B, C, D, and E are the five liver-specific viruses, each with its epidemiology, proclivity for chronicity, risk of liver consequences, and responsiveness to antiviral therapy. In the context of pregnancy, the mother's liver health, the influence of pregnancy on the clinical course of the viral infection, and the virus's or liver disease's effect on the growing newborn must all be taken into account.
References:
- Terrault, N.A., Levy, M.T., Cheung, K.W. et al. (2021). Viral hepatitis and pregnancy. Nat Rev Gastroenterol Hepatol 18, 117–130. https://doi.org/10.1038/s41575-020-00361-w
- El Jamaly, H., Eslick, G. D., & Weltman, M. (2021). Systematic review with meta-analysis: autoimmune hepatitis in pregnancy. Scandinavian journal of gastroenterology, 56(10), 1194–1204. https://doi.org/10.1080/00365521.2021.1953127
- Asafo-Agyei KO, Samant H. Pregnancy and Viral Hepatitis. [Updated 2021 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556026/
- (2020). Hepatitis: Preventing mother-to-child transmission of the hepatitis B virus. [online] World Health Organization. Available at: https://www.who.int/news-room/q-a-detail/hepatitis-preventing-mother-to-child-transmission-of-the-hepatitis-b-virus. (Accessed on 6th October 2021).
- (2020). Perinatal Transmission. [online]. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/hepatitis/hbv/perinatalxmtn.htm. (Accessed on 6th October 2021).
- Cui, AM., Cheng, XY., Shao, JG. et al. (2016). Maternal hepatitis B virus carrier status and pregnancy outcomes: a prospective cohort study. BMC Pregnancy Childbirth 16,87. https://doi.org/10.1186/s12884-016-0884-1
- Roberts, E. A., & Yeung, L. (2002). Maternal-infant transmission of hepatitis C virus infection. Hepatology (Baltimore, Md.), 36(5 Suppl 1), S106–S113. https://doi.org/10.1053/jhep.2002.36792
Further Reading
Last Updated: Oct 22, 2021