Melanoma is a health condition with a long history that dates back to early records in the 5th century BC.
Image Credit: Tatjana Bacina / Shutterstock.com
Ancient history
In approximately the 5th century BC, Hippocrates was the first to record a description of melanoma, which he described as melas, meaning dark, and oma, meaning tumor, in Greek.
There is some archaeological evidence of melanoma in the skeletons of pre-Columbian mummies in Peru, which have been radiocarbon dated to be approximately 2,400 years old, thus approximately the 4th century BC.
Initial practice and findings
John Hunter was the first man recorded to operate on a patient with melanoma, performing the first successful excision of a melanoma tumor in 1787. At the time, he did not know exactly what it was and described it as a “cancerous fungous excrescence.” It was not until many years later, in 1968, that the preserved tumor was examined under a microscope to determine that it was metastatic melanoma.
Rene Laenec was the first to distinguish melanoma as a disease separate from others in 1804, with the term melanose. In 1820, William Norris was the first to observe the heterogenic nature of some melanoma tumors. The term melanoma was ultimately introduced in 1838 by Sir Robert Carswell.
In 1826, Thomas Fawdington wrote that the medical profession was quite in the dark as to the remote and existing causes of melanoma. For this reason, it was necessary to confess the incompetency of knowledge at this time, leaving revelations about the governing principles of the disease to future investigators. At this time, anesthesia and antiseptic agents had not yet been introduced, and knowledge about DNA and the development of cancer did not yet exist.
Progression of knowledge
In 1844, Samuel Cooper was the first to formally acknowledge that advanced melanoma was untreatable and that “the only chance for benefit depends on early removal of the disease.” Even today, with continued research and development, this statement remains true.
In 1892, Herbert Snow expressed the benefits of removing the tumor and surrounding glands as a method of prophylaxis in the treatment of melanoma. He believed that the excision of the tumor alone was an ineffective treatment and, wherever possible, the lymph glands should be removed, as they are quick to receive the infective protoplasm.
In 1905, William Handley analyzed the lymphatic spread of secondary melanoma on a woman’s leg, which formed the basis of a case study for the disease. He suggested that the surrounding subcutaneous tissue and lymph nodes should be removed, which guided the surgical treatment for melanoma for the proceeding 50 years.
Etiology and genetic involvement
In 1956, Henry Lancaster made the initial connection between ultraviolet (UV) radiations from exposure to sunlight to an increased incidence of melanoma. This idea was supported by the work of Lancaster and Nelson, who demonstrated that the characteristics of the skin had an impact on melanoma development, which include:
- Skin color
- Texture
- Hair color
- Eye color
- Reaction to the sun
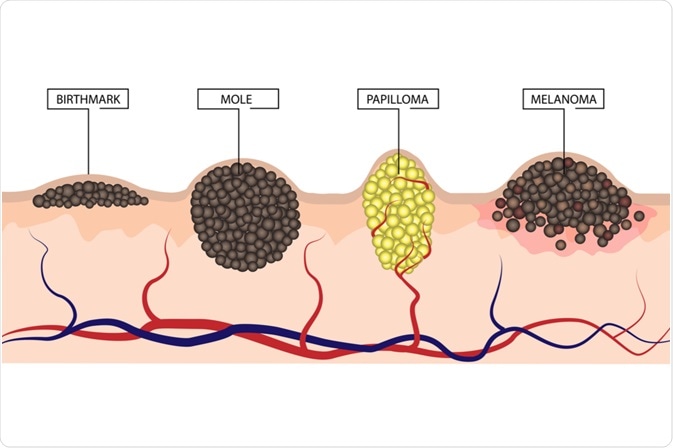
Image Credit: LiliiaKyrylenko / Shutterstock.com
The risk of melanoma was markedly increased in individuals with fair skin who were previously exposed to high levels of UV radiation, such as those residing in Australia and New Zealand.
Following the introduction of this classification of the various stages of disease progression, several medications were approved for use in the treatment of melanoma.
Current knowledge and future challenges
At this point in time, we have a relatively good understanding of melanoma, in that we know it is caused by exposure to UV radiation and results from the malignancy of melanocytes. It is understood that some individuals are at a higher risk of melanoma due to their specific skin characteristics, as well as polymorphisms in the melanocortin receptor-1 (MC1R) or CDKN2A genes.
However, the precise mechanism of the progression of a melanocyte into melanoma remains unknown and, as a result, methods of prevention are limited. This area is an appropriate subject for future research.
References
Further Reading
Last Updated: Jul 14, 2023