Monkeypox is a rare disease caused by the monkeypox virus, which is an orthopoxvirus from the same group of viruses as smallpox. Although naturally occurring smallpox has been successfully eradicated, monkeypox remains endemic in the forests of Central and Western Africa, with sporadic reports of human outbreaks and areas of endemic disease.
The disease can spread to people when they are either bitten or come in the contact with blood and body fluids of animals infected with monkeypox. The symptoms of the disease in humans are similar to those of smallpox, albeit usually milder. Accurate and rapid laboratory diagnostics is paramount in controlling an outbreak.
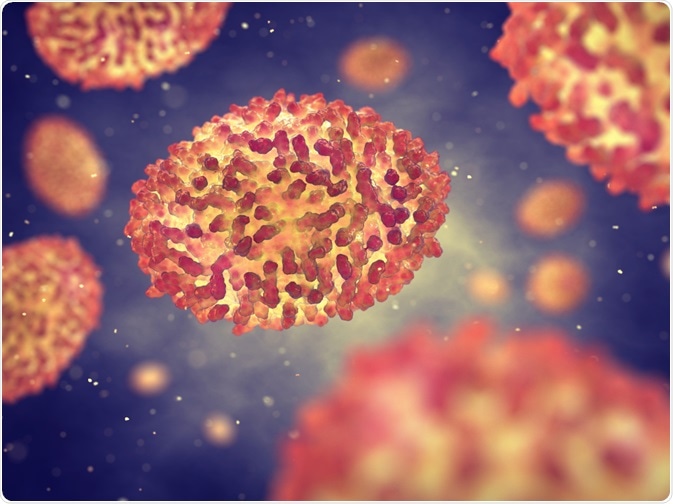 The monkeypox virus is an orthopoxvirus from the same group of viruses as smallpox. Image Credit: nobeastsofierce / Shutterstock.com
The monkeypox virus is an orthopoxvirus from the same group of viruses as smallpox. Image Credit: nobeastsofierce / Shutterstock.com
Modes of transmission
Monkeypox virus was once restricted to specific regions of Africa, but the environment of the disease has expanded, suggesting that human monkeypox infections may continue to intensify. The specifics of viral circulation in animal populations and the exact species that harbor this virus are not entirely known, although research and evidence point to rodents as a likely reservoir.
Transmission is believed to occur from an infected animal through a bite or via direct contact with saliva, respiratory excretions, lesion exudate or crust material. Abrasions in the mouth of individuals eating infected monkeys or squirrels also represent a route of transmission, and viral shedding via animal feces may represent another exposure source.
Even though human-to-human transmission of monkeypox is not so efficient, it did occur in up to 11.7% of household contacts of patients without prior smallpox vaccination. Primary routes are through direct contact and via respiratory droplet spread. Theoretical risk for airborne transmission is also present.
The longest uninterrupted sequential transmission events of human-to-human spread is considered to be six individuals, and clusters of such patients have been repeatedly described. Transmission in hospital settings has also been documented, which is potentially preventable employing standard type of precautions and (where applicable) vaccination.
Conditions that facilitate the occurrence of human cases of monkeypox include the constant circulation of the virus in wild animals in forests and agricultural areas surrounding human settlements, the use of meat of wild animals as an important source of animal protein, as well as close contact of humans with wild animals.
 The specifics of viral circulation in animal populations and the exact species that harbor this virus are not entirely known, although research and evidence point to rodents as a likely reservoir. Image Credit: Chanawat Phadwichit / Shutterstock.com
The specifics of viral circulation in animal populations and the exact species that harbor this virus are not entirely known, although research and evidence point to rodents as a likely reservoir. Image Credit: Chanawat Phadwichit / Shutterstock.com
Human cases and outbreaks of the disease
Initial nine outbreaks of monkeypox occurred between 1958 and 1968 in nonhuman primate colonies in laboratories and a zoo. No cases have occurred in animal handlers, and there were no cases reported in captive monkeys after 1968. At that time it was a novel orthopoxvirus, which was conveniently named "monkeypox virus".
Between 1970 and 1979, investigations of human monkeypox were underway in tropical rainforest areas of several central and western African countries following smallpox eradication activities. During this period, 54 cases of human monkeypox were confirmed in forested areas, and 80% of them were recorded in the Democratic Republic of Congo. Seven of the reported infections were fatal.
An active surveillance program conducted by the World Health Organization in the Democratic Republic of Congo found that 338 of the 404 recognized cases in Africa occurred between 1970 and 1986. In that same period, human monkeypox cases were also noted in the forests of the Central African Republic (6 cases), Liberia (4 cases), Nigeria (3 cases), Côte d’Ivoire (2 cases), Cameroon (1 case) and Sierra Leone (1 case).
Since 1981, most reported cases have occurred in the Congo Basin of Central Africa, which is still the area with the majority of human monkeypox infections each year. The case-fatality ratio in Central Africa in the 1980s was approximately 10% in non-vaccinated individuals, in contrast to no fatalities in cases occurring in West Africa due to a difference in virulence between the Central and West African strains of the virus.
In 2003, the first cases of human monkeypox in the western hemisphere were described after an outbreak was reported in Midwestern US (Illinois, Indiana, Kansas, Missouri, Ohio and Wisconsin) due to the importation of West African rodents from Ghana infected with monkeypox. This outbreak led to the understanding of the sanitary hazards resulting from the international trade of exotic animals.
Surveillance for human monkeypox cases in endemic areas still represents a challenge. Lack of resources, poor infrastructure, inadequate diagnostic specimens and cumbersome clinical recognition of monkeypox disease are just some of the challenges encountered by surveillance systems. Control of this illness primarily lies in health education aimed at changing the routine eating customs of the population at risk.
References
Last Updated: Dec 21, 2022