A mucocele is a mucus cyst produced by extravasation of salivary secretion due to the rupture of a salivary gland duct, or salivary retention within an accessory salivary gland, due to duct stricture or sialoliths. The mucocele appearance is highly characteristic in most cases, and diagnosis is made on clinical grounds.
The clinical diagnosis is based upon the findings of a soft, fluctuant, bluish-white to pinkish lesion which is dome-shaped, with an acute onset and often, a history of minor mechanical trauma preceding it. Fluctuation may be absent if the lesion has undergone some fibrosis, or is draining.
If necessary, other tests may be ordered, including a biopsy if there is any suspicion of malignancy. Ultrasound evaluation is very helpful in most cases because of the high fluid content of the cyst. If the origin and extent of the cyst are doubtful, CT or MRI scanning may help. If a ranula has grown large and is encroaching into the neck muscle, it may require scanning, for instance. Fine needle aspiration cytology (FNAC) with chemical and cellular analysis is helpful in the diagnosis of a ranula. A fine-needle aspiration biopsy (FNAB) may help rule out other lesions especially if the color or size are atypical.
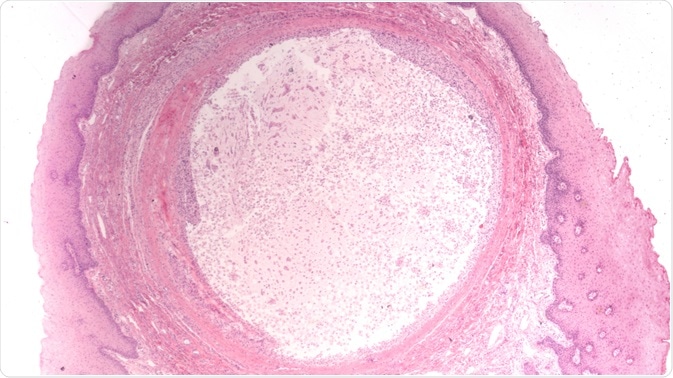 Microscopic image of a mucocele (mucus cyst). Image Credit: David A Litman / Shutterstock.com
Microscopic image of a mucocele (mucus cyst). Image Credit: David A Litman / Shutterstock.com
Management of mucoceles
In the majority of cases, a mucocele ruptures within a few days without any intervention being required. Healing is rapid in most cases, and the shallow erosion produced by the rupture is only mildly painful. Recurrence may occur if the salivary duct is not properly removed or if adjacent salivary glands are damaged. For this reason, and to prevent infection, the cyst should not be pricked or otherwise removed by the patient.
Excision of a recurrent or persistent mucocele is usually performed in one of the following ways:
- Surgical excision: this must be done with great care to avoid nerve damage to a branch of the lingual nerve, in case of a ranula, or nearby salivary gland damage which could cause recurrence.
- Cryosurgery which uses liquid nitrogen flowing through a probe tip to freeze the lesion
- Carbon dioxide laser to ablate the cyst
- Electrocautery to excise the cyst
Ranulas are usually removed using laser or cryosurgery, both the damaged gland and the mucus cyst itself.
Surgery for mucoceles
There is no clinical or management difference between the retention and extravasation mucoceles.
The most common mode of removal is surgical mucocele excision. This involves the removal of the cyst, the mucosa around it, and the glandular tissue until the muscular layer is reached. Just cutting through the top layer to allow drainage is not usually recommended because of the high recurrence rate. It is associated with the highest rate of complications, such as temporary paresthesia, fibrous scar formation, and hemorrhage. In all cases where the fibrous pseudocapsule wall is thicker than usual, the specimen must be sent for histopathological examination to ensure that it is not a neoplasm of the minor salivary gland.
Marsupialization, which means unroofing the cyst so that it can drain into the mouth, is adopted for larger mucoceles, especially ranulas, as it avoids deep dissection which could cause damage to the labial branch of the mental nerve. Small cysts should be completely excised, along with the minor glands at the periphery, and the wound sutured to achieve hemostasis and rapid healing.
Retention mucoceles need duct dilatation with a lacrimal catheter, in addition, to ensure that it drains salivary secretion properly.
Micromarsupialization is another technique that employs a thick silk suture passed through the lesion at the largest diameter and knotted. It is left in place for 7-10 days, within which time the cyst reduces and vanishes. It is used in small children, being less painful, simple, non-traumatic, and having a good success rate.
Other methods of excision
Carbon dioxide laser absorbs water efficiently and therefore is taken up by the cyst, leading to its vaporization while sparing adjacent structures. It has the additional advantages of precision, rapid action, excellent simultaneous hemostasis and absence of inflammation while healing.
Electrocautery and cryosurgery also help to ablate the lesion while sparing adjacent structures and achieving good hemostasis. All of these have the disadvantage of not providing a histological sample.
Intralesional injection of corticosteroids is also used to treat a mucocele. It is most useful when there are multiple mucoceles and separate surgical excision would be difficult.
Mucocele - Types, Clinical Features, Histopathalogic features & Treatment
Complications of mucocele treatment
Surgical excision is associated with the highest number of complications, which include:
- Recurrence in case of incomplete removal
- Injury of nearby nerves, salivary glands, or salivary ducts, during dissection, which may also lead to recurrence
- Hemorrhage
- Nerve injury in case of a ranula, involving the labial branch of the mental nerve
- Temporary paresthesia
References
Further Reading
Last Updated: Feb 25, 2021