India is currently fighting its second wave of COVID-19 while cases of rare and often fatal fungal disease mucormycosis are beginning to soar alongside this second surge of COVID cases. The infection, which has high mortality rates, is threatening the health of those across India where many regions are already struggling to handle the rise in COVID-19 cases.
Mucormycosis is challenging to treat, often this is exacerbated as patients commonly seek medical attention too late, once the infection has already begun to spread. First-line therapy usually involves anti-fungal treatments, however, because mucormycosis is notoriously difficult to cure, treatment strategies involve methods of early diagnosis, to catch the infection before it spreads.
There is also a focus on reversing the disease that underlies the infection, currently, COVID-19 is acting as the underlying disease for the rising cases of mucormycosis in India. Finally, doctors focus on surgical management of the fungal infection, the debridement of infected tissue is often vital to eradicating mucormycosis. Here, we discuss all three strategies.
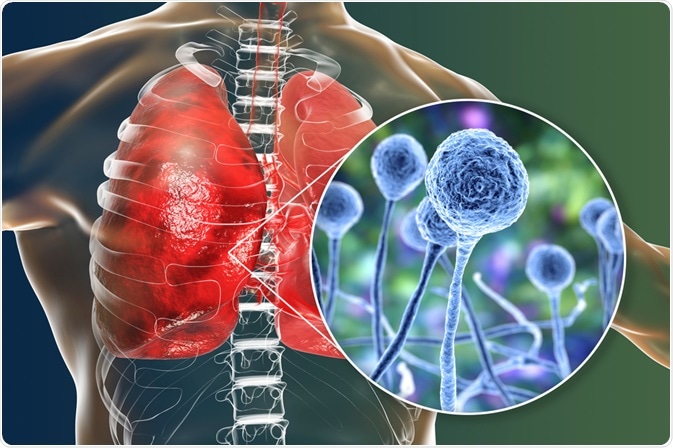
Mucormycosis. Image Credit: Kateryna Kon/Shutterstock.com
Early diagnosis of mucormycosis
The earlier patients begin receiving antifungal therapy, the better their chances of survival are. Recent evidence demonstrates that anti-fungal treatment initiated within the first five days following diagnosis significantly improves the patient’s chances of survival in comparison to those who begin therapy six or more days after diagnosis (83% vs 49%). Therefore, the efficacy of antifungal therapy, the key first-line treatment for mucormycosis, is heavily dependent on early diagnosis and initiation of treatment.
Unfortunately, there is a serious unmet need for effective and accessible diagnostic methods for mucormycosis, which impacts a physician’s ability to reliably diagnose mucormycosis apart from other potential diseases at an early stage. Currently, work is underway to establish a method of rapid diagnosis using quantitative polymerase chain reaction systems. However, until this is available, the most commonly used diagnostic tools are CT and MRI scans.
Unfortunately, both these strategies have their drawbacks. CT scans cannot distinguish between sinusitis and mucormycosis. MRI scans, while more sensitive, still require significant time for the scanning to take place and skilled professionals to read the results, which are subject to interpretation. Therefore, there remains a need for a rapid, reliable, and objective diagnostic tool for mucormycosis.
Anti-fungal therapy for mucormycosis
Once mucormycosis has been diagnosed, treatment with anti-fungal agents can begin. Early initiation of this treatment, as discussed above, is key for its success in preventing tissue from being infiltrated by the fungus, resulting in the need for disfiguring corrective surgery, and, ultimately, improving outcome and survival.
Usually, anti-fungal therapy for mucormycosis is based on polyene. Previously, amphotericin B deoxycholate (AmB) was the first choice of anti-fungal therapy for mucormycosis. Now, newer lipid formulations of AmB that are less nephrotoxic are favored as they can be administered at higher doses for longer periods.
In addition, treatment of mucormycosis with liposomal amphotericin B (LAmB) has been shown to be more effective than AmB (survival rate of 67% vs 39%). As a result, physicians now prefer to use lipid polyenes to treat mucormycosis, rather than AmB.
Treating the underlying disease
In combination with treating the patient with anti-fungal agents to address the infection, physicians also focus on treating the underlying disease that has allowed mucormycosis to develop. Immunosuppressive medications lower the immune response, which can give infections a better chance to establish themselves.
In the case of COVID-19-related mucormycosis, it is often the steroids used to treat the inflammation that lowers the immune response and allows the fungus to take hold. Effective treatment of the underlying disease, therefore, is key as it allows the administration of immunosuppressive drugs to stop.
Surgical management of mucormycosis
Blood vessel thrombosis and tissue necrosis are often the results of mucormycosis. This can prevent anti-fungal agents from penetrating the infected site, reducing their efficacy. Debridement of necrotic tissue, therefore, is often crucial for completely eradicating the fungal infection. Studies have found that surgery is associated with favorable outcomes in patients with mucormycosis.
In addition, a higher mortality rate has been demonstrated in patients who did not undergo surgical debridement of mucormycosis in comparison with those who did. Data also suggests that patients who do not undergo surgery are also more likely to suffer from increased disease severity than those who did undergo surgery. The timing and extent of surgery must be optimized to maximize patient outcomes.
Overall, mucormycosis is difficult to treat with generally poor outcomes and a high mortality rate. There is an unmet need for more effective and rapid diagnostic methods to allow for early diagnosis and initiation of treatment, which is key to improving patient outcomes. Current strategies involve early initiation of antifungal treatment, as well as addressing underlying diseases associated with the onset of mucormycosis, and finally, surgical debridement is also often crucial for improving patient outcomes.
Sources:
- Jeong, W., Keighley, C., Wolfe, R., Lee, W., Slavin, M., Chen, S., and Kong, D., 2019. Contemporary management and clinical outcomes of mucormycosis: A systematic review and meta-analysis of case reports. International Journal of Antimicrobial Agents, 53(5), pp.589-597. www.sciencedirect.com/science/article/abs/pii/S0924857919300020
- Skiada, A., Lass-Floerl, C., Klimko, N., Ibrahim, A., Roilides, E. and Petrikkos, G., 2018. Challenges in the diagnosis and treatment of mucormycosis. Medical Mycology, 56(suppl_1), pp.S93-S101. https://academic.oup.com/mmy/article/56/suppl_1/S93/4925966?login=true
- Spellberg, B. and Ibrahim, A., 2010. Recent Advances in the Treatment of Mucormycosis. Current Infectious Disease Reports, 12(6), pp.423-429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2947016/
Further Reading
Last Updated: May 20, 2021