A wide range of clinical trials has been conducted with the aim of improving our understanding of multiple sclerosis (MS) and discovering effective treatments for this disease.

Image Credit: DannyFalse / Shutterstock.com
What is MS?
MS is a chronic inflammatory disease that affects the central nervous system (CNS) and can lead to severe physical, neurological, and/or cognitive disabilities.
As the most prevalent neurological disability, MS is an autoimmune-mediated disorder that severely disrupts the myelin sheath surrounding the nerve fibers of the CNS. Some of the primary causes of myelin destruction in MS include focal T-lymphocytic and macrophage infiltrations, as well as oligodendrocyte death. The accumulation of these inflammatory cells and their products, as well as demyelinated axons, accumulate and form plaques throughout the CNS.
Pathogenesis
Although MS is heavily studied, the etiology and pathogenesis of this disease remain unclear. Research suggests that MS is caused by a genetic predisposition coupled with certain environmental factors; however, the exact cause of the condition remains a controversial topic.
Genetics of MS
A genetic predisposition towards the disease has been identified; however, several studies have shown that the risk of MS in patients with a family history of the disease depends on how much genetic information they share with the affected relative.
In fact, monozygotic twins, who have 100% genetic similarity with each other, only have about a 25% risk of MS. Comparatively, individuals who have 50% genetic similarities, such as dizygotic twins and first-degree relatives, will have a much smaller risk of MS that is within the range of 2% to 5%.
Within the human leukocyte antigen (HLA) region of chromosome 6 is several genes that have been associated with an increased risk of MS. These genes include HLA-DR2+, HLA-DQ6, DQA 0102 and DQB1 0602, HLA-DRB1, DR15, DRB1*1501, and DRB1*1503. Interleukin 7 (IL-7) and IL-2 receptor alpha are also two genes that are sensitive to MS.
Environmental factors
Several different environmental factors have been associated with the onset of MS, the most common of which include prior viral and/or bacterial infections, smoking, vitamin deficiency, diet, and exposure to ultraviolet (UV) radiation.
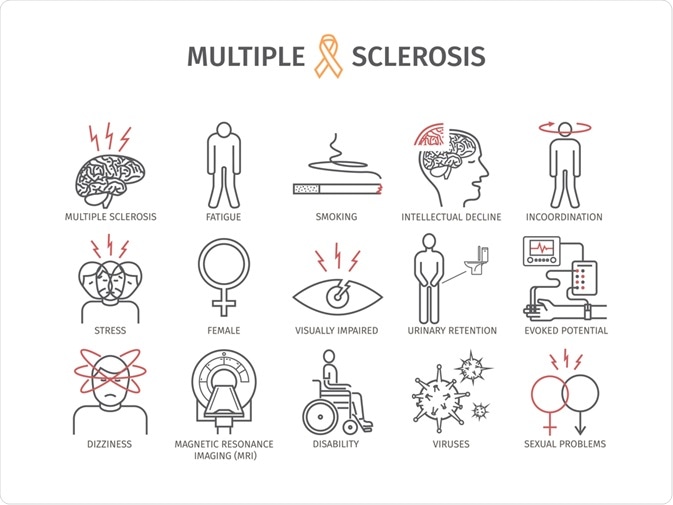 Image Credit: Prokopenko Oleg / Shutterstock.com
Image Credit: Prokopenko Oleg / Shutterstock.com
Viral and bacterial causes
It has been suggested that individuals who have been infected by Epstein Barr virus (EBV) during their lifetime might have a higher risk of developing MS. Other infections that have reported a positive association with MS include the human herpesvirus type 6 and mycoplasma pneumonia.
Smoking
The inhalation of nitric oxide (NO) and carbon monoxide (CO) through the smoking of cigarettes have both been linked to MS.
NO, for example, is a toxic soluble gas that is capable of damaging neurons and oligodendrocytes. More specifically, NO is associated with lipid peroxidation and mitochondrial damage, both of which can lead to oligodendrocyte apoptosis, axonal degeneration, and demyelination.
Previous studies have also found that CO can cause a variety of neurotoxic effects including myelin basic protein (MBP) degradation and axonal injury. In addition to blocking tissue oxygenation, CO can also induce an inflammatory response that activates microglia and the invasion of CD4+ lymphocytes into the CNS.
Vitamin deficiency and diet
Deficiencies in vitamins D and B12 are often associated with an increased risk of MS. Vitamin D, which includes cholecalciferol (D3) and ergocalciferol (D2), plays an important role in cell proliferation and differentiation, gene expression, the regulation of immunity, as well as the suppression of proinflammatory cytokines.
Therefore, the lack of vitamin D in the circulation prevents these processes from occurring normally, which can further contribute to the pathogenesis of MS. Vitamin B12 also plays an important role in regenerating certain components of the myelin shell; therefore, the lack of this vitamin can significantly impact the proper functioning of the CNS.
In addition to a diet that is low in these vitamins, diets that are high in animal fats have been associated with an increased risk of MS. Comparatively, a high intake of fish has been associated with a reduced risk of MS. A positive association between obesity in adolescent girls and MS risk has also been reported.
UV radiation
Studies have indicated that people exposed to an optimum amount of sunlight each day are less susceptible to MS. This may be because Vitamin D, which is produced in response to sunlight, stimulates the immune system in such a manner that it reduces the chances of MS.
Treatment advances
Although there is no cure for MS, several therapies have been approved for use in patients with MS. Each of these therapeutics has different mechanisms of action, routes of administration, efficacy, and safety profiles.
Disease-modifying therapies
Disease-modifying therapies (DMTs) that are used in the treatment of MS include immunomodulatory agents such as interferon beta and glatiramer acetate, both of which have been available as injectables for several years. These agents work by inhibiting the activation of immune cells, reducing the production of proinflammatory cytokines and the activity of matrix metalloproteinases, as well as increasing the secretion of anti-inflammatory cytokines.
Although the safety and efficacy of these injectable therapies have been confirmed through long-term studies, the use of injectables has reduced over the past several years as alternative DMTs with improved tolerability and efficacy profiles have been developed.
Some of the different oral DMTs that are associated with improved efficacy include several selective sphingosine 1-phosphate (S1P) receptor modulators. In addition to these S1 receptor modulators, several additional oral DMTs have been developed with different mechanisms of action include pyrimidine synthesis inhibitors. Overall, the oral medications that have been developed for MS treatment are well tolerated and reduce several adverse effects that are often associated with injectables, such as the increased risk of infection.
Stem cell therapy
Adult Stem Cells Heal Multiple Sclerosis Patient
There are several goals associated with stem cell therapy in the treatment of MS, some of which include replacing damaged cells, increasing the regulation of nerve growth factors, as well as reducing the circulation of inflammatory cytokines and apoptotic factors. Additionally, stem cell therapy offers a promising treatment option for the subset of MS patients who do not respond to any of the aforementioned DMTs.
Autologous hematopoietic stem cell transplantation (AHSCT) has been widely studied for its utility in treating treatment-resistant relapsing MS. Recent studies have shown that after transplant, between 80% and 87% of patients remain relapse-free for at least 5 years. Moreover, several clinical trials have demonstrated similar high rates of relapse-free survival, as well as improved disability and magnetic resonance imaging (MRI) measurements.
Overall, these findings suggest that AHSCT is an effective therapy for MS patients with active and relapsing disease. Current research is underway to evaluate how AHSCT compares with some of the best available therapies for MS.
References
- Ghasemi, N., Razavi, S., & Nikzad, E. (2017). Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy. Cell Journal 19(1); 1-10. doi:10.22074/cellj.2016.4867.
- Goldschmidt, C., & McGinley, M. P. (2021). Advances in the Treatment of Multiple Sclerosis. Neurologic Clinics 39(1); 21-33. doi:10.1016/j.ncl.2020.09.002.
Further Reading
Last Updated: Jul 24, 2021