By Prof Madhukar Pai
Cepheid Inc., produces Xpert MTB/RIF, which is an automated, fast test for TB using molecular diagnostics. Compared to the standard test for TB in developing countries, sputum smear microscopy, it is considerably more accurate.
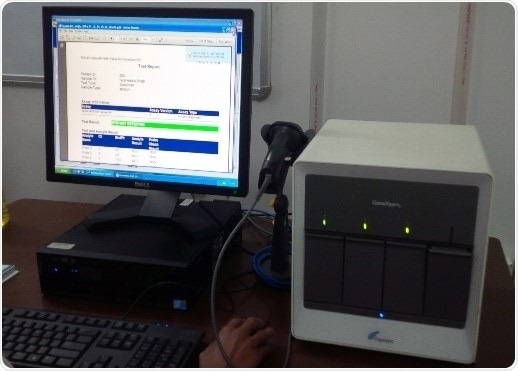
In an hour and a half, Xpert provides accurate tuberculosis detection as well as recognition of rifampicin resistance, an important drug used to combat TB. The GeneXpert system is simple to use and automated, meaning that testing can be finished outside of reference labs.
The large expenses associated with molecular tests cause this type of diagnosis to be rare in high TB burdened nations due to the need for reference labs with highly trained technologists. Xpert is the first diagnostic tool to disrupt these obstacles.
By merging drug-susceptibility and detection testing in the same test, Xpert has helped detect many more patients with multidrug-resistant tuberculosis (MDR-TB) than expected. Thus, Xpert is a pathfinder for universal drug-susceptibility testing, a crucial constituent of the End TB Strategy by WHO. The success of Xpert has also been appealing to several companies, enticing them to consider entry into the TB market.
The progress of Xpert was sustained by numerous contributors including NIH and the Bill & Melinda Gates Foundation. This lead to a concessional, subsidized pricing of $9.98 per cartridge. But this price only applies to the public sector in qualified high burden countries. Xpert was endorsed by WHO in 2010, and since then, over 16 million subsidized cartridges have been purchased and used in high TB burden countries.
Unfortunately, even in resource-limited countries, eligibility is restricted to the private sector for the subsidized $9.98 per test price. For the private sector in developing countries, higher prices for devices and reagents are set by manufacturers, costs such as import duties add additional costs, and intermediaries, distributors and labs all impose margins of their own. This results in much higher prices for patients in the private sector.
Benefits of private sector access to subsidies
In many countries, the private health sector is a dominant provider of medical care. In 12/22 countries with the greatest TB burden, the private sector is a major source of TB care. These countries are Cambodia, Philippines, Afghanistan, Kenya, Vietnam, Indonesia, Nigeria, Pakistan, India, Bangladesh, Kenya, Uganda and Myanmar. In these countries, even underprivileged TB patients prefer to seek care from private health-care providers.
In these settings, studies have shown that deferred diagnosis and misdiagnosis have been found to be major difficulties. Further, patients frequently switch between public and private sectors, and doctors also tend to have dual practices in both sectors.
If TB is to be diagnosed in a timely manner and accurately, we must consider patient pathways to care and appreciate care seeking patterns. Irrespective of where patients go for medical care, we have to safeguard that they have access to patient-centric, quality TB diagnosis and therapy.
What are patients paying for Xpert in the private sector in high burden countries?
We recently published a study on this issue (Puri L et al. Lancet Global Health 2016). We wrote to TB experts in 12 countries largely within the private sector, and enquired whether Xpert was available in the private sector within their country. We also asked them to gather price figures from private labs that did offer Xpert.
Results of our survey showed that in half the countries, there was no private health facility offering Xpert testing. In the other 6 countries, the average cost payable by private patients was US$68·73, with a range of $30·26–$155·44.
Our survey showed that Xpert availability in the private sector is low, and, with some exclusions, private sector patients pay for a lot for this test. Taken together, we think these issues could negate the potential impact of new diagnostic technologies.
IPAQT model in India
We found one notable exception to the above pattern. The lowest average price could be found in India, via labs in the IPAQT network (Initiative for Promoting Affordable and Quality TB Tests).
IPAQT is an enterprise coordinated by theClinton Health Access Initiative (CHAI), in New Delhi, India. Labs that join IPAQT offer several WHO-approved diagnostics at lower prices. IPAQT labs provide Xpert at a standard price of INR 2000 ($30·26), compared with a $52.82 average in the rest of country’s private sector.
IPAQT now includes 115private labs that are accredited in its network as of February, 2016. These labs obtain a concessional price for Xpert, liquid cultures and line probe assays. In return for the right to use the public sector concessional pricing for equipment and reagents, these labs have agreed to pass on price discounts to patients, by not charging any more than a clearly agreed maximum price, informing TB cases to the public sector, and contributing in external quality assurance programmes. More than 250 000 TB tests have been completed by IPAQT labs since its introduction in 2013.
The future of access to TB Diagnostics
We need a plan, to safeguard that good diagnostics can be obtained by all patients with suspected TB. Such an access policy must draw on numerous methods. For example, it could include the the private sector in existing and upcoming pricing arrangements.
For a panel debate, see the below video:
8th FIND Symposium at Union World Conference 2015
Reproduction of IPAQT-like models in further countries could be tried out. Another approach is to design public-private partnerships that permit privately managed patients to be tested in public labs. Innovative schemes such as usage of vouchers and subsidies by private provider interface agencies, and social businesses to cross-subsidise TB tests alongside more profitable tests are all worth trying.
Lastly, since TB is a disease of the poor, diagnostic companies need to rethink their strategy and adopt mass-market rather than premium pricing models for tuberculosis products.
About Prof Madhukar Pai, MD, PhD
Prof Madhukar Pai, MD, PhD is a Canada Research Chair in Epidemiology & Global Health at McGill University, Montreal. He is the Director of McGill Global Health Programs, and Associate Director of the McGill International TB Centre.
Disclaimer: This article has not been subjected to peer review and is presented as the personal views of a qualified expert in the subject in accordance with the general terms and condition of use of the News-Medical.Net website.
Further Reading
Last Updated: Dec 30, 2022