Noroviruses are positive-sense, non-enveloped RNA viruses, which are a leading cause of viral gastroenteritis and a common cause of outbreaks in institutional settings. Infections with these viruses are difficult to prevent and control, as their genome recombines or mutates readily, and new variants can emerge every few years to become the dominant strains in a certain period.
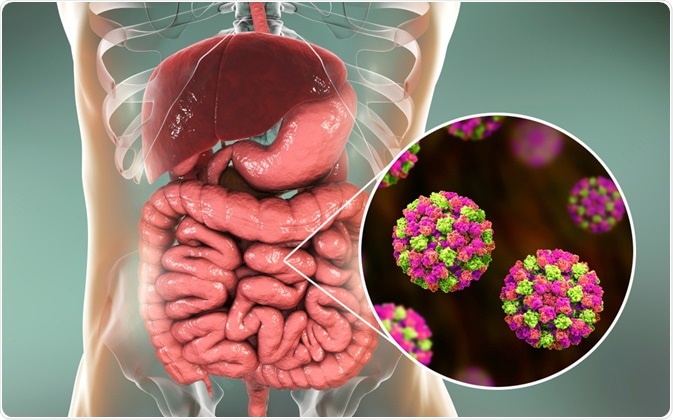
Image Credit: Kateryna Kon / Shutterstock.com
The majority of norovirus outbreaks are caused by the GII.4 genotype, which has been the predominant circulating virus since 1995. The development of molecular-based diagnostic methods has provided better insight into the epidemiological impact of noroviruses, which is important to identify trends for the detection, prevention, and control of the disease.
Transmission routes
Several routes of norovirus transmission have been identified due to a myriad of well-documented outbreaks. In general, the person-to-person spread represents the primary mode of transmission in outbreaks. This remains true for endemic cases of norovirus infection, which are primarily facilitated by the low infectious dose of between 18 and 1000 virus particles.
However, foodborne transmission can also play an important role, often as a result of contamination by an infected food handler, which highlights the fecal-oral route of transmission. In addition, several waterborne outbreaks have been described, and there is indirect evidence of potential airborne transmission, such as in explosive vomiting that occurred during the disease.
In most cases, different modes of transmission are responsible for outbreaks. One example is when a food handler becomes infected via person-to-person transmission in his or her home, and then subsequently contaminates a food product, leading to a common source outbreak. This, in turn, may progress further through person-to-person transmission or environmental contamination.
Transmission of Norovirus
Epidemiology of norovirus
It is estimated that approximately 200,000 people die each year from norovirus infections, especially in the developing world. Outbreaks affect health care facilities worldwide, with the potential to cause a massive disruption in their ability to provide care, substantial economic loss, and mortality in vulnerable patient groups.
Humans are considered to be the only host for human noroviruses, although recent detection of related noroviruses in pooled stool samples from calves and swine has hinted at the possibility of zoonotic transmission. As interspecies transmission has been documented for other animal caliciviruses, which are known for their wide host range, animals as a potential reservoir for human infections remains a significant public health question.
Norovirus excretion patterns may have an important role in the spread of the virus. Virion excretion can occur after all the major symptoms have disappeared, but norovirus RNA excretion can happen even before the onset of symptoms. Furthermore, the excretion can continue for long periods of time, especially in immunocompromised individuals.
Prevention
Efficacious prevention of norovirus outbreaks has proven particularly challenging, as outbreaks that begin with a single common exposure to a contaminated source can swiftly spread by person-to-person contact. After that, stopping the outbreak requires colossal efforts to adequately clean the environment.
Key preventive measures include personal hygiene, enteric precautions, and decontamination of environmental surfaces. Assays and tests that have been employed in specific outbreaks for the direct detection of viruses in contaminated food and water are now being adapted to routine screening of food or water.
Studies testing vaccines based on virus-like particles are just beginning to emerge. Even though the need for universal vaccination remains unknown, target groups in sensitive situations like the elderly in nursing homes may benefit from a vaccine. In addition, vaccination of food handlers may help to prevent large-scale foodborne outbreaks.
References
Further Reading
Last Updated: Mar 11, 2023