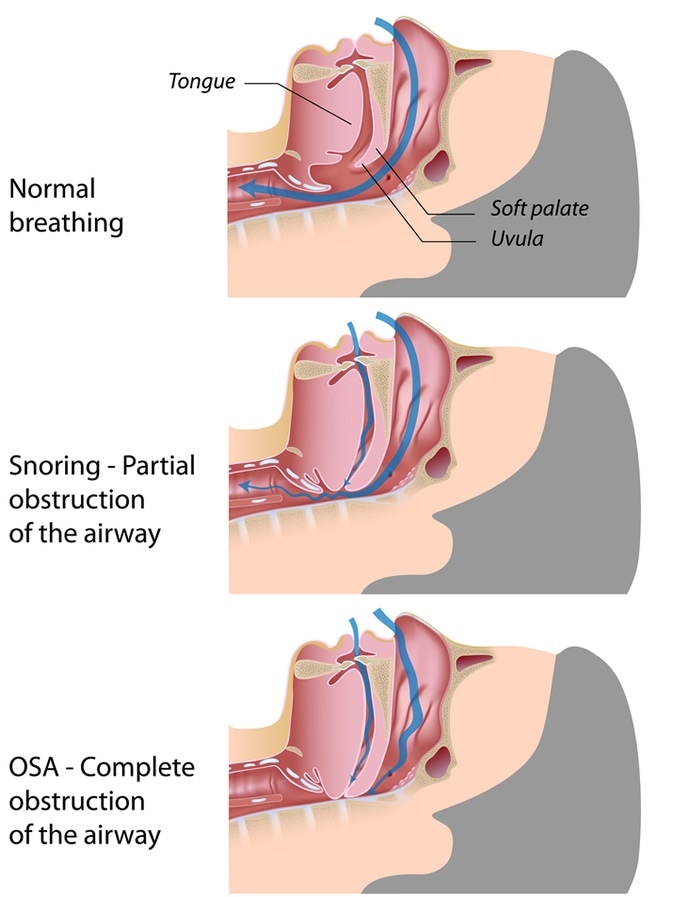
Obstructive sleep apnea (OSA) is a medical condition that occurs when one stops breathing periodically during sleep. The brief pause in breathing is most often due to obstruction within the airway.
Obstructive Sleep Apnea - Image Credit: Alila Medical Media / Shutterstock
Between 1 – 10% of children are believed to be affected by OSA, and those commonly affected are 3 – 6 years of age. A typical patient is one with Down syndrome or another congenital ailment.
A child experiencing an episode of OSA will appear as if she or he is trying to respire, but there is notably no exchange of pulmonary gases.
Some children may waken during the process so that the resulting increase in airway muscle tone can return air entry to normal. Repetitive OSA cycles during the night may have significant impact on the quality of a child’s sleep.
Obstructive Sleep Apnea in Children - Children's Hospital New Orleans
Causes
Enlarged tonsils and lymphoid glands in the upper respiratory tract are the most common causes of OSA in children.
Hypertrophy of the tonsils, which may occur during an infection, may completely block the nasal passage. This blockage makes it extremely difficult or nearly impossible to breathe through the nose.
During sleep, muscle tone decreases, leading to tissues collapsing to some extent, which is responsible for sleep-induced narrowing of the airway. This narrowing is made worse by the presence of enlarged glands.
Other causative OSA factors are craniofacial anomalies, neuromuscular diseases and, though rare, tumorous growths in the upper airway. Obesity may also be a cause, but this is more common in the adult population.
Signs and Symptoms
Children with OSA may have a spectrum of signs and symptoms that are not uniformly seen in all affected patients.
Some common symptoms, however, include breathing through the mouth, snoring loudly, excessive daytime sleepiness and periodic pauses in breathing during sleep.
OSA patients may have social and academic difficulties and they may be more hyperactive during the day than their peers. Moreover, these children may be aggressive or irritable at times.
Children at the age of 5 or older may also experience enuresis, which is involuntary urination while sleeping.
Furthermore, there may be paradoxical movement of the rib-cage, frequent periods of waking up during the sleep cycle, and diaphoresis, or profuse sweating.
Parents will often note the apneic episodes themselves. Children with OSA commonly have a failure to thrive, because, it is hypothesized, the work required to breathe during sleep causes massive caloric expenditure.
Diagnosis and Treatment
A complete medical history is necessary in addition to physical examination as the initial steps to diagnosing OSA. Sleep specialists, otolaryngologists and, if applicable, pulmonologists are consulted.
Overnight sleep tests at a specialized center are conducted to identify the problem during sleep. Other diagnostic tests that may be employed include chest X-rays in order to ascertain if there are problems within the lungs or large airways.
Treating OSA depends largely on the cause. In the case of enlarged tonsils, surgical removal may be recommended. Other candidates for surgery are children with craniofacial abnormalities.
If surgery would not be beneficial or helpful, then continuous positive airway pressure (CPAP), via a mask, can be used to keep the airway open during sleep. Obese children will need to lose weight as part of the management process.
In other instances, as for neurological or other primary causes of sleep apnea, pharmacotherapy, behavioral modification, and education may be required.
Further Reading
Last Updated: Feb 27, 2019