Spinal deformities in children may be the result of many conditions, such as congenital malformation of the spinal column, disorders of the neuromuscular system or trauma. They may be progressive in which case their severity increases with age, leading to restrictions of pulmonary growth, nerve function and heart pumping capacity.
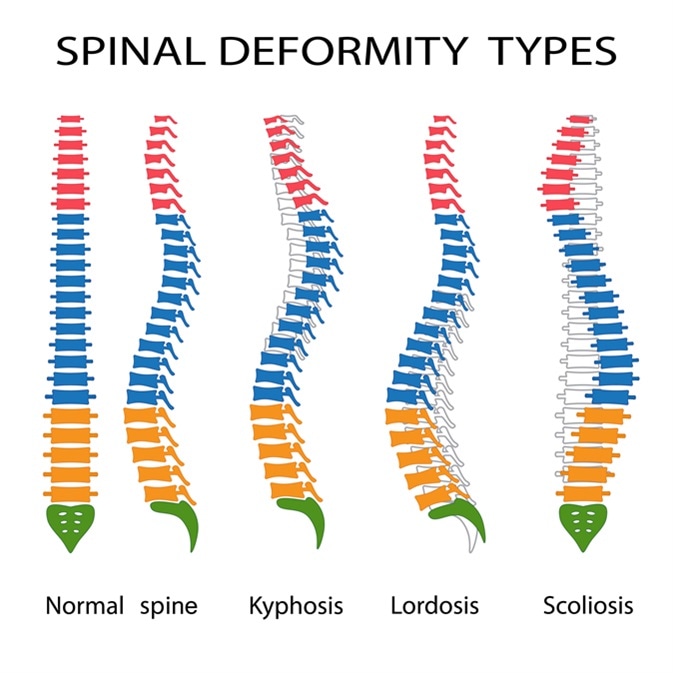
Illustration of spinal deformity types. Kyphosis, lordosis and scoliosis. Image Credit: Neokryuger / Shutterstock
Classification
The classification of pediatric spinal disorders has undergone several metamorphoses, such as that by King and Lenke et al. Their usefulness always depends on how well they are able to recognize the impact of the root condition, as well as the predicted effect on normal growth of the child, the natural history, and the extent of disability that is possible and preventable by appropriate management.
Pathological systems of classification focus upon the reason for the deformity, such as abnormal spine development, neuromuscular disease leading to unbalanced strains on the developing cord, or other disorders of spinal column formation. Other systems classify them by the age of onset, whether infancy, early childhood, or adolescence. The most commonly used systems deal with the structural changes that are present, such as the degree of curvature, the direction and rotation of the spine, as well as other anatomical results of the deformity. These structural systems offer the most help with clinical management and are the most reliable with respect to the response to treatment.
The most common spinal deformities in childhood include scoliosis (curving of the spine to one side), kyphosis (curvature of the spine in the backward direction), spondylolysis (stress fractures in the lower back) and spondylolisthesis (one vertebra slips over another).
Diagnosis and treatment
Pediatric spinal deformities can be diagnosed based on the patient history, family history, and complete physical examination. Clinical findings, such as unequal height of shoulders, tilted head or pelvis, difficulty in breathing, limping or back pain, may be found. Imaging modalities are very useful in diagnosing these conditions, such as X-rays, CT, MRI and DEXA scans. Most spinal deformities require only observation to ensure that they are not progressing.
The management of pediatric spinal deformities depends on the extent to which they have been allowed to interfere with normal growth. Growth spurts soon after birth, as well as during adolescence, can aggravate the malformations. These have to be anticipated when planning corrective surgery to prevent undue shortening of the spine.
Treatment may be non-surgical or surgical. Non-surgical treatment includes brace application and spinal casts. Surgical correction includes fusing a segment of the spine with screws and rods to arrest or reverse the deformity. In children who are still growing, growing rods are used, which can be expanded every few months to keep up with the increase in spinal length. Once growth is complete spinal fusion is performed.
References
- https://www.ncbi.nlm.nih.gov/pubmed/15766220
- https://www.ncbi.nlm.nih.gov/pubmed/14713581
- https://www.emoryhealthcare.org/
- http://thejns.org/doi/pdf/10.3171/foc.2003.14.1.4
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4940247/
- http://www.chop.edu/conditions-diseases/spinal-deformities
Further Reading
Last Updated: Dec 29, 2022