Pheochromocytoma is a catecholamine-producing tumor that originates from chromaffin cells of the adrenergic system, most commonly in the adrenal medulla. There are two main steps in the diagnosis of pheochromocytoma: biochemical demonstration of excessive catecholamine secretion and radiological localization of the causative tumor.
 Image Credit: Shidlovski/Shutterstock.com
Image Credit: Shidlovski/Shutterstock.com
Patients with pheochromocytoma may come to medical attention due to their hypertension (which is paroxysmal in approximately one-third of patients but can also be sustained) or because of the clinical features that stem from the increased secretion of catecholamines (i.e. epinephrine and norepinephrine).
In any case, the diagnosis should be suspected in patients with one or more of the following:
- The onset of hypertension at a young age
- Resistant or labile hypertension
- Hypertensive response during anesthesia, surgery, or angiography
- Paroxysmal and self-limiting episodes of typical adrenergic symptoms
- Incidentally discovered adrenal mass
- Family history of pheochromocytoma
- Familial syndrome predisposing to catecholamine-secreting tumors
Biochemical investigation
In the past, biochemical screening involved measurement of urine excretion of catecholamines and total metanephrines in the 24-hour urine. Today, the diagnosis of pheochromocytoma has been made simple by significant developments in the assays that are used to both detect and quantify catecholamine levels in the blood and urine.
Nevertheless, as fractionated plasma metanephrines are considered products of catecholamine metabolism within pheochromocytomas, they can also be detected in blood with high sensitivity (i.e. approaching 100%). Such improved sensitivity is a result of the persistent production of metanephrines that contain a high concentration of catechol-O-methyltransferase.
Moreover, as levels of these metabolites evince a universal feature of pheochromocytoma – a continuous metabolism of catecholamines within the tumor – the measurement of plasma metanephrines is thought to be diagnostically superior to measuring only serum catecholamines.
False-positive results can arise due to the presence of other medical conditions, most notably obstructive sleep apnea, and medications such as selective serotonin-reuptake inhibitors or SSRIs that can cause the elevation of metanephrines; hence patients should stop taking all medications that can possibly interfere with the results prior to testing.
Chromogranin A is a major secretory protein present in the chromaffin granules and a very effective tumor marker that can improve the sensitivity of diagnostic testing and long-term follow-up for pheochromocytoma. Clonidine suppression and glucagon stimulation tests have been studied, but are seldom required and have not been validated in the diagnosis of childhood pheochromocytoma.
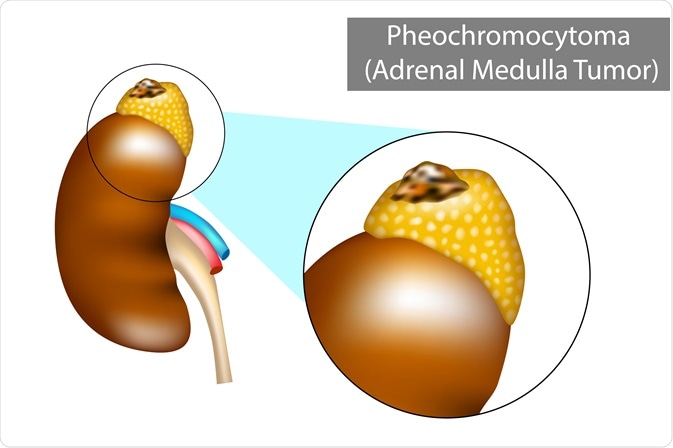 Image Credit: Sakurra/Shutterstock.com
Image Credit: Sakurra/Shutterstock.com
Radiographic studies
Upon establishing the biochemical diagnosis of catecholamine excess, radiographic studies are undertaken in order to pinpoint the exact location of the tumor. The test of choice is cross-sectional imaging (either by using computed tomography or magnetic resonance imaging) of the abdomen and pelvis, which is followed by imaging studies of the neck and chest. In children, there is also a possibility to apply abdominal ultrasound.
Nuclear scintigraphy with radioiodine is then used to confirm the catecholamine-secreting nature of the tumor, but it can also be utilized to localize tumors that were not seen with computed tomography or magnetic resonance imaging. Once again, attention should be given to medications that patients are taking, as even over-the-counter decongestants can decrease the uptake of radiotracers.
Such functional imaging also has its place in ruling out extra-adrenal pheochromocytoma, as well as any metastatic pheochromocytomas. There is also some research on the use of nuclear magnetic resonance spectroscopy as a modality that complements the findings of computed tomography or magnetic resonance imaging.
References
Further Reading
Last Updated: Feb 21, 2023