The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has affected 188 countries across all continents. The rapid spread of the SARS-CoV-2 virus has meant that both healthcare facilities caring for those with COVID-19 and facilities working to test people for the virus have often become overwhelmed, and delays in getting results from SARS-CoV-2 testing makes containing the virus more difficult.
 Image Credit: JHDT Productions/Shutterstock.com
Image Credit: JHDT Productions/Shutterstock.com
How SARS-CoV-2 is currently tested
The current tests for SARS-CoV-2 include viral testing and antibody testing.
Viral tests also called nucleic acid and antigen tests, use samples taken from the nasal passages or mouth to see whether the SARS-CoV-2 virus is present in the respiratory system. Viral tests show whether a person is currently infected with COVID-19.
A negative test means that the person was not infected at the time the test was taken, but they may have since become infected if they did not quarantine or self-isolate while waiting for their test results.
An antibody test checks to see if a person has had a SARS-CoV-2 infection in the past. It is not a widely available test, and is not effective in everybody, as it is not guaranteed that a person will produce antibodies against SARS-CoV-2 after an infection.
Antibody tests do not tell a person if they are immune to further infection from SARS-CoV-2, or whether a person can spread the virus to other people. An antibody test uses a blood sample to test for coronavirus antibodies.
A person infected with SARS-CoV-2 can be pre-symptomatic (infected and will experience symptoms at later stages of infection) or asymptomatic (infected but will not experience symptoms at any stage of infection). This may mean that infected individuals may not know they are infected and will unknowingly spread the virus to other people, and will not undertake quarantine measures to control the spread.
As a result, it is very important that asymptomatic people, including people who have been in contact with a person with a confirmed case of SARS-CoV-2 infection, are tested as efficiently as possible.
However, testing for those people who believe they have been in contact with people who have been infected with SARS-CoV-2, or who believe they may be infected themselves, is under immense pressure worldwide.
Using saliva for SARS-CoV-2 tests
Saliva is used to test for several viral infections already, including dengue, Ebola, and Zika virus, as well as yellow fever. SARS and MERS are also tested with saliva samples.
The whole saliva collected from the mouth contains glandular secretions, gingival crevicular fluid, serum, expectorated airway surface liquid, mucus, epithelial and immune cells from oral mucus and the upper airways, as well as oral microbes and viruses.
It is not yet known why SARS-CoV-2 may be present in saliva. It could be that material from the nasopharyngeal epithelium drains into the mouth to then be mixed with saliva. Additionally, SARS-CoV-2 could also be present in saliva if it infects the salivary glands that then produce saliva infected with the virus.
Studies have found that the SARS coronavirus targeted epithelial cells lining the salivary glands in a particular species of monkey that was infected with the virus, which may suggest that tests could target these cells early on in a case of infection. SARS-CoV-2 from blood plasma may also enter the saliva through crevicular fluid from the periodontal tissues.
It could be that SARS-CoV-2 could be more easily detected in the saliva in certain people, as the site of infection may be different between individuals. The main sites of infection are the nasal, oral, pharyngeal, and respiratory tracts. This means that tests may better pick up on SARS-CoV-2 infections in people who were infected via the oral tract.
A meta-analysis found that the test sensitivity for SARS-CoV-2 was 91% for saliva testing. For nasopharyngeal swab (NPS) tests, the sensitivity was found to be 98%. Alternatively, other studies have found saliva to be more sensitive than nasopharyngeal or nasal swabs.
It is difficult to determine which test is more sensitive, and therefore more effective than the other. This is because false negatives can occur, which may skew the results when comparing saliva and NPS tests. Additionally, studies used vastly different methods to collect saliva, which meant that the saliva collected may have included fluid from different areas of the respiratory and oral tracts and as such, may have included SARS-CoV-2 traces from areas other than the saliva.
This same meta-analysis concluded that drooling could be the best way to achieve the greatest sensitivity. It is also safer than nasopharyngeal and oropharyngeal swabbing, as potentially infected swabs do not have to be exposed to the air while being transferred from the patient to containers.
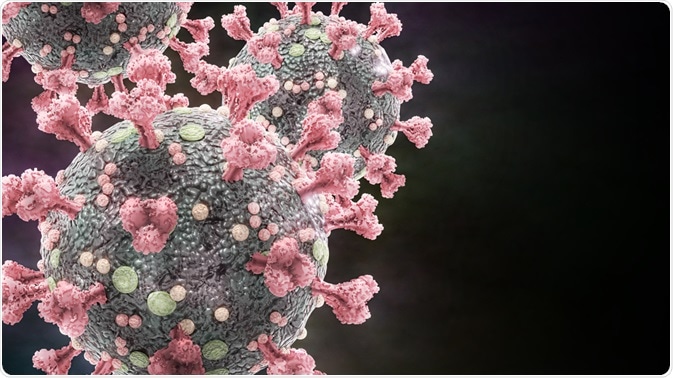 Image Credit: Dotted Yeti/Shutterstock.com
Image Credit: Dotted Yeti/Shutterstock.com
What is pooled testing?
Pooled testing is a technique in which samples from multiple people are combined and tested together. This method of testing can significantly improve efficiency and mean that more people can be tested for SARS-CoV-2 infection, making more effective use of the limited testing resources and personnel available.
If a positive test is found in a pool of samples, the samples are then tested to see which one is positive. Pooled testing is most efficient in places in which the prevalence of SARS-CoV-2 is low. This is because pooled tests that return negative results do not need to go through additional, individual testing to identify the positive sample.
There is an upper limit to the efficiency of pooled testing. If the prevalence of SARS-CoV-2 increases significantly, more and more pooled tests will need additional individual tests to identify positive samples. This means that a testing facility would eventually be doing more testing with pooled testing methods as additional tests for each pool would be necessary in a large number of cases.
However, there are limitations to pooled testing, which has been used since the 1940s. Pooled testing can be less sensitive than individual tests because the SARS-CoV-2 viral RNA, which is the target for the test, can be diluted in the mixture of samples that may not have any SARS-CoV-2 RNA present.
However, studies have stated that pooled testing can detect positive samples in pools of five samples, and studies from Israel, Germany, and the USA have stated that pools of 32 or possibly even 64 samples can still detect positive infections with additional polymerase chain reaction (PCR) amplification cycles.
Recent studies such as a large-scale pooling of 133,816 samples by Barak et al. suggest that the efficiency and sensitivity of SARS-CoV-2 tests are high, and support the use of large-scale testing.
Cross-contamination and specimen tracking can also be a problem for pooled testing, as human error and the chance of mishandling samples when working with multiple pooled samples at a time increases.
What Is Pooled Testing? | Quick Learner
Summary
Increased capacity for and efficiency of testing for SARS-CoV-2 is of great importance as the pandemic continues to spread. Pooled testing is a technique that can greatly increase the number of samples that get tested as it involves combining separate samples and testing them together. However, there is a risk of sample dilution with pooled testing.
Saliva may also be equally as effective as samples taken from the nose, for instance, and saliva can be easier and safer to collect from people.
Pooled saliva testing is a promising method for testing for SARS-CoV-2 and may allow people to collect their samples, greatly reducing the human resources needed to carry out testing, reducing pressure on healthcare and testing facilities.
References
Further Reading
Last Updated: Mar 19, 2021