Urinary tract infections (UTIs) are a severe public health problem that are caused by a range of different pathogens. When the infection migrates to the upper urinary tract or is seeded there via blood, both the pelvis and parenchyma of the kidney become inflamed. This condition is then characterized as pyelonephritis.
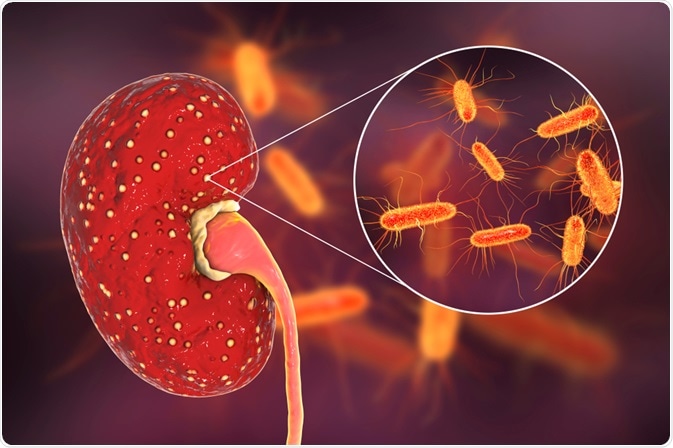
Image Credit: Kateryna Kon / Shutterstock.com
What is pyelonephritis?
Pyelonephritis can occur at any age; however, it often peaks during infancy, particularly in girls, the childbearing years for women, and the elderly, especially in men with prostate pathology. The risk factors in these groups include a relatively short urethra in infant girls, urinary tract obstruction by the enlarging uterus during pregnancy, and chronic obstruction that occurs as a result of prostatic hyperplasia.
Clinical features
The clinical manifestations of pyelonephritis can be highly variable. Classic symptoms of pyelonephritis include a sudden onset of chills, fever (body temperature of 38 °C or greater), and unilateral or bilateral flank pain with costovertebral tenderness. These signs are usually accompanied by dysuria, urinary frequency, and urgency.
Note that none of these symptoms are reliable for determining the precise anatomic level of infection. In addition, gastrointestinal symptoms can be also present in acute pyelonephritis – namely abdominal pain, diarrhea, nausea, and vomiting. Each of the aforementioned signs can therefore confound the diagnosis.
Children younger than two years of age may only present with high fever without symptoms related to the urinary tract. Other findings in these younger patients include poor feeding, abdominal pain and/or lethargy. Older children can present with fever, chills, emesis and/or flank pain, in addition to the typical signs of pyelonephritis of dysuria and urgency.
Approximately one-third of frail elderly patients with acute pyelonephritis have no fever, and may not exhibit other classic manifestations of the disease. In fact, up to 20% of elderly patients will this condition will instead experience predominant symptoms that are pulmonary and/or gastrointestinal in nature.
In contrast to acute pyelonephritis, chronic pyelonephritis represents a progressive process. The chronic state of this condition most frequently presents insidiously as progressive renal failure, often with hypertension. It is estimated that anywhere between 11% to 20% of end-stage renal disease is a result of chronic pyelonephritis.
Establishing a diagnosis
Medical history and adequate physical examination represent the most helpful tools for establishing an accurate diagnosis of acute pyelonephritis. Still, to confirm the diagnosis, laboratory tests such as urinalysis and urine culture are employed. Urine specimens are obtained by a midstream clean-catch technique, which is standard practice for obtaining a useful specimen.
Laboratory findings of the urine sample will typically include pyuria, bacteriuria, granular or leukocytic casts, and a positive urine culture. Hematuria may be present in individuals with cystitis and pyelonephritis. Blood tests may show elevated erythrocyte sedimentation rate, elevated CRP levels, and/or leukocytosis with a neutrophilic shift.

Image Credit: angellodeco / Shutterstock.com
Positive blood cultures that grow the same organism as cultured from the urine are sometimes found, most often in hospitalized patients. It should be noted, however, that there is no evidence a correlative blood culture will indicate a more complicated course of the disease in otherwise healthy patients with pyelonephritis.
Imaging studies are sometimes required to confirm a clinical diagnosis of pyelonephritis. More specifically, an ultrasound can easily detect the presence of obstruction, as well as demonstrate characteristic findings that are suggestive of acute pyelonephritis. Computed tomography (CT) is more sensitive than ultrasonography at spotting the condition; however, this imaging technique requires radiation exposure and typically requires the use of an intravenous contrast agent.
Other disorders that may arise from or mimic acute pyelonephritis should be considered before arriving at a definitive diagnosis. The differential diagnosis of this condition can include cholecystitis, appendicitis, pelvic inflammatory disease, lower lobe pneumonia, perforated viscus, and the prodrome of herpes zoster. Chronic pyelonephritis also has non-specific morphology and can be the result of numerous diverse etiologic factors.
References
Further Reading
Last Updated: Sep 25, 2022